Two sets of meta-analyses were performed with the abstracted data. First, the specified outcome measures were compared for patients taking inhaled corticosteroid vs leukotriene modifier therapy. Second, the impact (before vs after) of each treatment initiation was compared for each outcome.
Assessment of statistically significant differences between meta-analysis results was performed with the Student t test, with an Α of .05. Charges were used in the included studies as proxies for costs. These costs were inflated to 2000 values by using the medical care component of the consumer price index before inclusion.
Results
We identified 49 documents and reviewed them for inclusion in the meta-analysis; 6 (12.2%) met the inclusion criteria (Table 1). Five were retrospective cohort studies; only 1 study was identified as a prospective trial comparing inhaled corticosteroid and leukotriene modifier therapies and including results on resource use or medical care costs.16,17,22-25 All 6 studies were performed with support from GlaxoSmithKline.
Forty-three documents were excluded due to 1 or more of the following criteria: lack of primary results (9 documents, 21%); did not contain resource use rate or cost outcomes (22 documents, 51%); did not provide at least 6 months’ worth of data on resource use or cost outcomes (5 documents, 12%); did not meet the defined inclusion and exclusion criteria (primarily studies not including both inhaled corticosteroid and leukotriene modifiers or those restricted to patient clinical subgroups; 10 documents, 34%); or did not define the number of patients included in the study (1 document, 3%).
Because few studies presented data on the specified outcomes, we were unable to assess asthma-specific costs for subcategories of resource use. Too few studies included data on hospitalization costs (either asthma-specific or overall) to include in the analysis. Therefore, meta-analysis was performed on overall (ie, all causes) emergency department, pharmacy, and total medical care costs.
TABLE 1
Characteristics of studies included in the meta-analysis
| Duration (mo) | |||||
|---|---|---|---|---|---|
| Study | LOE* | Before therapy | After therapy | Treatment (N) | Comparison (N) |
| Oates and Gothard22 | 2b | 9 | 9 | Inhaled corticosteroids (546)† | Leukotriene modifiers (152)‡ |
| Pathak et al23 | 2b | 9 | 9 | Fluticasone propionate (284) | Leukotriene modifiers (497)‡ |
| Stanford et al24 | 1b | - | 6 | Fluticasone propionate (271) | Montelukast (262) |
| Stempel et al16 | 2b | 9 | 12 | Fluticasone propionate (602) | Zafirlukast (309) |
| Stempel et al17 | 2b | 9 | 9 | Fluticasone propionate (559) | Montelukast (382) |
| White et al25 | 2b | 9 | 9 | Inhaled corticosteroids (1305)† | Leukotriene modifiers (109)‡ |
| *LOE, level of evidence. For an explanation of levels of evidence. | |||||
| †Results were presented for all inhaled corticosteroids combined. | |||||
| ‡Results were presented for all leukotriene modifiers combined. | |||||
Primary analysis
The primary objective of this study was to evaluate the impact of inhaled corticosteroid and leukotriene modifier treatment on the mean annual hospitalization rate. Four of the 6 included studies contained information on hospitalization rate for each treatment. Results from the primary analysis are presented in Table 2.
Patients taking inhaled corticosteroids had a significantly lower annual rate of hospitalization than did patients taking leukotriene modifiers (2.23% vs 4.30%, respectively; P<.005). The absolute risk reduction was 2.07% (number needed to treat=48 for 1 year).
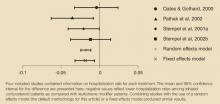
The difference in annual hospitalization visit rates for each study in the primary analysis is presented in the Figure, where negative values reflect lower hospitalization rates among patients taking inhaled corticosteroids than among those taking leukotriene modifiers. Two studies16,23 had statistically significant differences in hospitalization rates, whereas the differences in the other 2 studies were not statistically significant (P<.05). Combining studies with the use of a random effects model (the default methodology for this analysis) or a fixed effects model produced similar results. The Q statistic indicated no significant heterogeneity (P=.43).
TABLE 2
Meta-analysis results for inhaled corticosteroid vs leukotriene modifier therapy*
| Inhaled corticosteroid vs leukotriene modifier patients † | ||||
|---|---|---|---|---|
| Inhaled corticosteroids | Leukotriene modifiers | Absolute difference | Relative difference | |
| Annual asthma hospitalizations‡ | 2.23% (1.69-2.78) | 4.30% (3.53-5.07) | -1.79% (-2.45 to -1.14) | -42.88% (-55.95 to -29.80) |
| Annual rate of visits to the emergency department due to asthma§ | 6.19% (4.84-7.53) | 7.74% (6.30-9.19) | -1.53% (-1.78 to -1.28) | -21.35% (-25.31 to -17.38) |
| Total annual costs of visits to the emergency department | $93 (38-148) | $73 (52-94) | $21(-17 to 59) | 1.00% (-38 to 40) |
| Total annual drug costs§ | $807 (548-1065) | $1062 (812-1312) | -$258 (-308 to -208) | -27.20% (-33.2 to -21.3) |
| Annual asthma-related cost‡ | $882 (613-1150) | $1393 (1143-1643) | $513 (-392 to -634) | -38.01% (-47.4 to -28.8) |
| Total annual cost | $5254 (4474-6033) | $7140 (4970-9311) | -$1918 (-3509 to -327) | -17.20% (-30.9 to -3.5) |
| *Data are presented as mean (95% confidence interval). | ||||
| †Absolute and relative differences were determined from meta-analyses of the absolute and relative differences for each included study. | ||||
| ‡Inhaled corticosteroid vs leukotriene modifier significant at P<.05. | ||||
| §Inhaled corticosteroid vs leukotriene modifier significant at P<.005. | ||||
FIGURE
Difference in hospitalization rates (mean, confidence interval)
Secondary outcomes
Results of secondary analyses for 5 study outcomes (annual visits to the emergency department due to asthma, total emergency department costs, total drug costs, total asthma-related costs, and overall total cost) are presented in Table 2.
Mean annual rates of visits to the emergency department and total annual drug costs were significantly higher for patients taking leukotriene modifiers than for those taking inhaled corticosteroids (P<.005 for each). Patients taking leukotriene modifiers had lower annual costs for visits to the emergency department than did those taking inhaled corticosteroids, although this difference was not statistically significant. The higher rate and lower cost of emergency department visits for patients taking leukotriene modifiers suggest that medical resources were used less at each visit as compared with those for patients taking inhaled corticosteroids.