- Advanced age, positive family history, smoking, hypertension, and Caucasian ancestry are risk factors consistently associated with age-related macular degeneration (ARMD).
- With older patients, suspect ARMD if vision has decreased or if Amsler grid testing reveals scotoma or metamorphopsia (C).
- Refer any patient with suspected ARMD for an ophthalmology consultation (C).
- Lifestyle modifications, vitamin supplementation, and low-vision aids can slow or mitigate the effects of ARMD (A).
Age-related macular degeneration (ARMD) is no longer the ocular death sentence it once was. Therapies are improving and becoming more widely available.
Though everyone over 40 should have an ophthalmologic exam every year or 2, many patients that may routinely see their primary care physician will not consult an ophthalmologist until a problem manifests (see Demographics of ARMD). With simple, in-office testing described in this article, you can help alert patients to the need for ophthalmologic follow-up.
Age-related macular degeneration (ARMD) is a progressive eye disease that can result in the loss of the center of our field of vision due to damage to the macula, the most important portion of the retina. It is the leading cause of central vision loss in people over the age of 50 years in the United States1 and the resulting functional loss can be devastating. Over a 5-year time span, it is estimated that 1 in 3 people over the age of 70 years will develop signs of ARMD2 and that 315,000 Americans over the age of 74 years will develop signs of advanced ARMD.3 Since the risk of ARMD increases with age,1 the number of patients with this disease will increase as our population grows older.
5 Consistent risk factors
Several large, population-based studies have identified age, family history, smoking, hypertension, and Caucasian ancestry as risk factors consistently associated with ARMD.4 Other risk factors such as atherosclerosis, ultraviolet (UV) exposure, farsightedness, increased body-mass index, and cataracts4-6 have been suggested, but not consistently proven to increase risk.
The risk of developing ARMD increases with age.1 According to the Framingham Eye study, a person between the ages of 65 and 74 has a 6% chance of exhibiting ophthalmoscopic evidence of ARMD. For those 75 or older, the chances are almost 20%.1,7
The Beaver Dam Eye Study and Rotterdam Study looked at families with ARMD and found an odds ratio as high as 10:1 for siblings7,8 and 6:1 for the offspring of ARMD patients.7 Combining these risk factors, a person who lives to be 85 and has a first-degree relative with ARMD has a 48% chance of developing clinically detectable ARMD.7
Smoking and hypertension also correlate strongly with ARMD.4,6 Patients who have ARMD and continue to smoke are 3.6 times more likely to progress to the end stages of the disease with severe functional compromise. Even when patients quit smoking, the risk remains elevated for the next 20 years.9 Studies of ARMD and systemic hypertension show an odds ratio for clinically detectable dry ARMD at 2:1 for patients with a systolic reading of 160 mm Hg or greater, and an odds ratio of 4:1 for wet ARMD if the diastolic reading is greater than 95 mm Hg.10,11
Diagnosing ARMD
Though a dilated fundus exam remains the gold standard for diagnosing ARMD, other in-office diagnostic tools are also available.
Specific clues in the history
In addition to inquiring about a family history of ARMD, ask patients if they have difficulty recognizing faces or if words seem to disappear while reading. ARMD patients may also notice that telephone poles appear crooked.
Testing visual acuity
With the patient wearing a current pair of reading glasses, test one eye at a time in good lighting with a near vision card at 12 to 14 inches from the patient’s face. Though many disorders can cause decreased vision, a reading worse than 20/30 in an elderly patient could indicate undiagnosed ARMD. If the patient has noticed a recent decrease in vision, an immediate ophthalmology referral is indicated. If near vision has gradually worsened, referral is needed but perhaps not as urgently.
Amsler grid test for earlier diagnosis
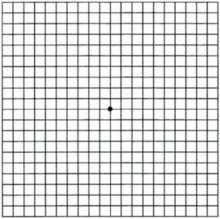
Amsler grid testing can detect ARMD (as well as other macular diseases) at a much earlier stage than can visual acuity testing alone. The grid (FIGURE 1; for a printable version, go to www.jfponline.com) is read with one eye at a time at a distance of 12 to 14 inches with reading glasses under good lighting conditions. Instruct the patient to focus only on the center dot in the grid and to view the remainder of the grid with peripheral vision and without looking around. If the patient reports that lines are missing (known as a scotoma) or appear wavy (known as metamorphopsia), the test is positive and prompt referral is indicated. The location of the distorted or missing lines corresponds closely with the location of the macular lesion.
FIGURE 1
Amsler grid
Patients with known ARMD can monitor their disease by performing this test once a day. This grid is shown actual size; a printable version is found at www.jfponline.com.