A 48-year-old Caucasian man comes to your office with redness and blurring of vision in his right eye that started the day before. For 3 weeks, he has had a productive cough with sputum, chills, and low-grade fever. Conjunctival injection is obvious. The view through the cornea is hazy, and there is a creamy white, layered settlement in the anterior chamber (FIGURE 1).
Q: What do you suspect may be causing his ailment?
FIGURE 1
Blurry vision in right eye
The patient has a layer of pus (hypopyon) in the anterior chamber of his right eye; the cornea is also cloudy.
Additional medical history
- The patient’s medical history reveals nothing significant.
- He has sustained no recent trauma to the eye.
Surgical history
- The patient had surgery to repair an umbilical hernia, and orthopedic surgery on his left elbow and ankle.
Family history
- His mother has chronic obstructive airway disease; his father has hypertension.
Social history
- The patient used cocaine about 20 years ago.
- He has abused alcohol, and is currently participating in an outpatient alcohol rehabilitation program.
- He is unemployed.
Review of systems
- Findings from other systems are unremarkable.
Physical examination
- The patient is alert and oriented.
- Temperature is 38.6°C (101.5°F), heart rate is 103 bpm, respiratory rate 20, blood pressure 114/57 mm Hg.
- Oxygen saturation is 95% on room air.
- Lungs: normal air entry bilaterally with a few crackles in right upper lung field.
- Heart: regular heart sounds, diastolic murmur in left lower sternal border.
- Abdomen: soft, nontender, nondistended, no organomegaly, and normal bowel sounds.
- Extremities show no significant edema.
Q: What are your next steps?
You request an immediate ophthalmology consultation, which confirms that visual acuity in the right eye is limited to light perception. The patient’s left eye exam is normal. In the slit-lamp examination of the right eye, the vitreous view is obscured by hypopyon and corneal haziness. Hypopyon signals inflammation of the anterior uvea and iris. Hypopyon can occur with such noninfectious problems as corneal ulcer, Behçet’s disease, systemic lupus erythematosus, sarcoidosis, and lymphoma/leukemia; and with endophthalmitis or panophthalmitis due to bacterial or fungal infection.
Based on the patient’s clinical presentation, you diagnose endogenous endophthalmitis, start treatment empirically with intravenous (IV) vancomycin, ceftriaxone, and moxifloxacin, and hospitalize him for further workup.
Endophthalmitis: A medical emergency
Endophthalmitis is a bacterial or fungal infection of the vitreous or aqueous humor of the eye.
The exogenous form occurs with direct inoculation of an organism into the anterior chamber, following penetrating or blunt trauma to the eye, insertion of a foreign body, rupture of the conjunctival bleb, cataract surgery (usually within 1 week of surgery), or intraocular lens implantation.
Endogenous endophthalmitis results from microbial seeding of the vitreous or aqueous humor during bacterial or fungal septicemia. The endogenous form accounts for just 2% to 16% of all cases of endophthalmitis.1-3 It is also known as metastatic endophthalmitis. Most of these infections arise suddenly, and it is a vision-threatening condition that should be managed as an ophthalmologic emergency.
Q: What additional tests would you order?
- The white blood cell count is 22,000/mcL; hemoglobin, 15.3 g/dL; hematocrit, 45.4%; platelets, 158,000/mcL; neutrophils, 8800/mcL; and bands of 10%.
- Basal metabolic panel is normal.
- Electrocardiogram is normal.
- Chest x-ray film shows right upper lobe infiltrate with minimal pleural effusion (FIGURE 2).
FIGURE 2
Posterior-anterior chest x-ray
The patient has consolidation in the right upper lobe with minimal pleural effusion on the right side.
Expanding the investigation
You consult an infectious disease specialist, who recommends continuing the antibiotics you’ve prescribed until blood culture results are available. Subsequent results are positive for Streptococcus pneumoniae with pansensitivity. The patient also undergoes transthoracic echocardiography, revealing a 9-mm mass on the aortic valve with associated severe aortic valve regurgitation and mild mitral valve regurgitation. The patient is transferred to the coronary care unit within 12 hours of his admission.
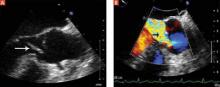
Surgery is scheduled immediately. A pre-operative transesophageal echocardiogram (FIGURE 3) confirms earlier findings and additionally reveals a small mitral valve vegetation. At surgery, the aortic valve is resected and replaced; a perivalvular abscess is drained.
Given culture results of S pneumoniae with pansensitivity, IV vancomycin is discontinued postoperatively, and IV ceftriaxone and oral moxifloxacin are continued for 6 weeks and 2 weeks, respectively. The ophthalmologist had also injected vancomycin into the vitreous; vitreous culture was not performed. At 6 weeks follow-up, the patient is blind in his right eye. He has also developed sensorineural hearing loss in his left ear, and has finished a course of steroids prescribed by an ear-nose-and-throat specialist.
FIGURE 3
Aortic valve vegetation, regurgitation
Transesophageal echocardiography image shows a vegetation on the coronary cusp of the aortic valve (A) and significant aortic valve regurgitation (B).