•Analyze P wave axis, morphology, and timing for help in diagnosing narrow QRS complex tachycardia. C
•Review the modes of onset and termination for clues to the specific type of tachycardia, including features such as the rate of acceleration and the response to medication and the Valsalva maneuver. C
•Compare a baseline 12-lead EKG with one taken during an episode of tachycardia, looking for clues to the mechanism of the arrhythmia. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Sinus tachycardia educational video for patients
Courtesy of: WirelessDx
Go to http://www.wirelessdx.com/sinustachycardia.htm

Narrow QRS complex tachycardias—rhythms with a rate >100 beats per minute (bpm) and a QRS duration <120 ms—are frequently encountered in both inpatient and outpatient settings. Therapeutic strategy ranges from simple reassurance to acute inpatient intervention, depending on the specific arrhythmia.
Early and accurate diagnosis is paramount to avoid unnecessary testing, ensure timely management, and prevent complications and long-term adverse outcomes. While most narrow QRS complex tachycardias are easily diagnosed, some pose a diagnostic challenge.

This review can help. We start with a summary of the various types of narrow QRS complex tachycardias, accompanied in some cases with 12-lead electrocardiogram (EKG) strips. Next, we highlight key characteristics to consider in the differential and provide an algorithm to help you zero in on the diagnosis.
Narrow QRS complex tachycardias: What you’ll find
Narrow QRS complex tachycardias fall into 2 broad categories: those that are sinus node-generated, and those that are not. Here’s a look at both.
Sinus node-generated tachycardias
Sinus node tachycardia (FIGURE 1), the most common arrhythmia,1 is an appropriate response to physiologic or emotional stress or disease processes. It is defined as a heart rate >100 bpm with the presence of P waves of normal sinus morphology on a 12-lead EKG.
FIGURE 1
Sinus tachycardia
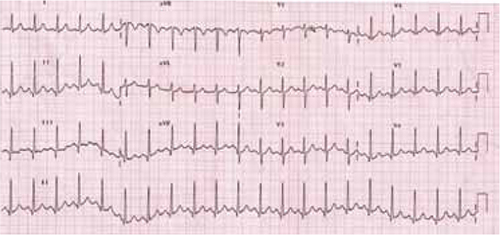
The P waves show normal sinus morphology. Note superior-to-inferior axis with positive P deflections in leads II, III, and aVF.
Inappropriate sinus tachycardia is a nonparoxysmal arrhythmia with a resting daytime heart rate >100 bpm (or an average heart rate >90 bpm over a 24-hour period), normal P wave morphology, and an exaggerated response to physical activity.2,3 What distinguishes it from simple sinus tachycardia is the disproportionate degree of the arrhythmia to the level of physiologic stress.
Inappropriate sinus tachycardia is a diagnosis of exclusion, established only after other reversible pathologic or pharmacologic causes of tachycardia, such as hyperthyroidism, pheochromocytoma, infection, or theophylline toxicity, have been ruled out. Possible mechanisms may include autonomic dysfunction with increased cardiac sympathetic or reduced vagal output.4
Paroxysmal orthostatic tachycardia syndrome (POTS) is an abnormal sinus tachycardia response to an upright position.5,6 It is diagnosed by a heart rate ≥120 bpm or an increase ≥30 bpm within 5 minutes of standing up or being on a tilt table, with simultaneous development of orthostatic symptoms, such as dizziness, light-headedness, or even syncope, without the corresponding drop in blood pressure. Symptoms usually resolve after the patient assumes a supine position. The presentation may overlap with that of inappropriate sinus tachycardia, although patients with POTS usually develop autonomic symptoms such as constipation, tremor, or heat/cold intolerance, as well.7,8
Sinus node reentry tachycardia is a paroxysmal tachycardia with a normal P wave on a 12-lead EKG. The paroxysmal nature of the arrhythmia and a positive response to atropine and vagal maneuvers, as well as identification by electrophysiologic studies, differentiate this condition from inappropriate sinus tachycardia.9
Nonsinus node-generated tachycardias
Focal atrial tachycardia (FIGURE 2) is caused by an automatic, triggered, or microreentrant mechanism that can be localized to a specific area of atrial tissue.10 The diagnosis can often be made by a careful review of the EKG, which will reveal P waves that differ from those of the sinus beat.11 This can be tricky, however, as a P wave on a 12-lead EKG from a focal point close to the sinoatrial node may resemble that of a normal sinus rhythm.
FIGURE 2
Focal atrial tachycardia
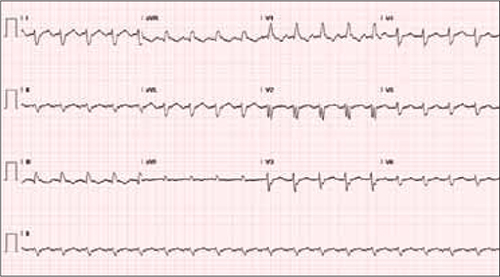
The P waves differ from those of the sinus beat. Note the positive P wave in lead aVR.
The atrial rate associated with this condition can vary from 120 to 300 bpm, depending on the focus, and may be associated with variable degrees of atrioventricular (AV) block. The crista terminalis in the right atrium and pulmonary vein ostia are frequent origins of focal atrial arrhythmias.12,13

