Statistical analyses
Each primary care site was asked to enroll subjects until 80 positive cases were identified from among all sites. The clinical laboratory site tested a minimum of 30 positive and 30 negative cases. The primary endpoint was the percentage of agreement (overall and within positive and negative cases separately) of results from both methods. Delta-over-baseline (DOB) enrichment values below 2.4 per mil were deemed negative and values greater than or equal to 2.4 per mil were deemed positive. The predicate reference method was gas isotope ratio mass spectrometry. Equivalence was defined by the percentage of agreement for positive and negative cases based on gas isotope ratio mass spectrometry results of at least 95%, and the lower limit of the 95% confidence interval was based on a percentage of agreement of at least 90% for positive cases.
Results
The primary care centers enrolled 258 subjects and the clinical laboratory enrolled 64 subjects, for a total enrollment of 322. The subjects’ mean age was 41.5 years (range, 18–70 years), with 88 black non-Hispanics, 106 Hispanics, 92 whites, 32 Asian/Pacific Islanders, and 4 other ethnic groups. There were 215 women and 107 men. Approximately 18% had active or previous gastrointestinal ailments, including previously diagnosed H pylori infection (11%) and peptic ulcer disease (3%).
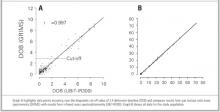
There was excellent agreement between methods (Table), with an overall agreement of 99% (95% confidence interval, 97.3–99.7). Two subjects were excluded from the analysis of the primary and secondary endpoints because 1 or both assay values were missing. The data showed close correlation between methods among all sites (Figure). Evaluation by the personnel who performed the tests and analyses indicated that the office procedure was easy and nonintrusive.
There were 3 disagreements between the results obtained with the devices, 1 from the gastroenterology site and 2 from the clinical laboratory site. All results were near the cutoff value.
TABLE
Comparison of results between IRMS and GIRMS*
| GIRMS, % | |||
|---|---|---|---|
| IRMS, % | Negative | Positive | Total |
| Negative | 1 | 115 | 116 |
| Positive | 202 | 2 | 204 |
| Total | 203 | 117 | 320 |
| *Overall agreement, 99.1% (95% confidence interval, 97.3–99.7); positive agreement, 98.2% (95% confidence interval, 94.2–99.7); negative agreement, 99.5% (95% confidence interval, 97.3–99.9). | |||
| Kappa statistic = 0.98. | |||
| GIRMS, gas isotope ratio mass spectrometry; IRMS, infrared mass spectrophotometry. | |||
FIGURE
Comparison of results between 2 methods of analysis of 13CO2 breath sample enrichments
Discussion
13C-urea breath testing is an accurate diagnostic method for the detection of active H pylori infection12,19-21 and point-of-care assessment of curative therapy. This study confirmed the hypothesis that the infrared instrument is an easy to operate alternative to the original sendout analyses. Rapid turnaround allows for decisions regarding therapy to be made at the time of care. The currently approved UBT in the United States does not require fasting from solid food for longer than 1 hour.
Noninvasive alternatives to UBT include serology and stool antigen testing. Serology assays cannot discriminate between active and recent past infections. Stool antigen testing requires patient compliance with specimen collection and is a sendout test. In general, although studies using pretreatment stool antigen tests have shown sensitivity and specificity comparable to those of histology or UBT, it has become evident that there can be considerable lot-to-lot variation in stool antigen tests.22 The most likely explanation is that the polyclonal serum used for the capture antibody is obtained from rabbits and thus difficult to standardize.23 Stool antigen testing has also proven to be less reliable when used soon after the end of therapy, and it is now generally recommended that one must wait 6 or 8 weeks after therapy when using the stool antigen test to confirm eradication. For example, a recent study had a false negative rate of 12.5% (95% confidence interval, 1.5–33).24Recent recommendations are that the UBT is preferred where available.4
The US Food and Drug Administration recently cleared the UBiT-IR300 instrument for use with the commercial 13C-UBT. The costs of the UBT are but a fraction of those of endoscopy, not including indirect patient costs. Office-based testing has a separate reimbursement for testing, and overall the costs appear less than those of the stool antigen test. Economic impact studies comparing the tests are planned. Office-based infrared analysis for 13C makes near-patient or point-of-care UBT and analysis practical and should make accurate diagnosis of active H pylori infection readily available.
Acknowledgments
The authors thank the clinical study coordinators, including Ms Rebecca Garza, Ms Flora Godard, and Mr Zachary Patton for their conscientious efforts.