Who is at risk for DHF?
Risk factors for the development of DHF include advanced age, female sex, hypertension, and coronary ischemia. Approximately 50% of those older than 70 years who have heart failure have preserved LV function.14-16 In a large epidemiologic study of elderly patients with heart failure, women were twice as likely as men to have preserved LV function.17 In examining post-myocardial infarction (MI) patients with heart failure, women and those with smaller infarctions were also more likely to have preserved LV function (odds ratio=1.97; 95% confidence interval [CI], 1.27–3.07).18
Hypertension is a well known cause of left ventricular hypertrophy (LVH), which is a causal mechanism for DHF.19,20 Levy et al, in a study of 5143 subjects from the original Framingham Heart Study participants and Framingham Offspring participants, found that hypertension predated the development of heart failure in 91% of cases among patients in this cohort.21 In this sample, hypertension also carried the greatest population-attributable risk for the development of heart failure of all risk factors considered (39% in men and 59% in women). Hypertension also had the highest prevalence of all risk factors in this study (60% in men and 62% in women). Untreated hypertension leads to an increasing incidence of LVH and associated diastolic dysfunction. Increased LV mass and stiffness cause noncompliance and abnormal relaxation of the ventricular wall leading to increased diastolic pressures.4,19-21
Coronary ischemia can also cause diastolic dysfunction.20 Data from the Framingham Heart Study indicate that the prevalence of MI was 10% in hypertensive men and 3% in hypertensive women.21 MI is a well known precursor of LV systolic dysfunction; however, the relationship to diastolic dysfunction is less clear. Although the prevalence of MI was associated with a 5- to 6-fold risk for heart failure in Framingham subjects, after adjustment for age and other risk factors, fewer than half of the patients who subsequently developed heart failure had a history of MI. This finding supports the role of untreated hypertension in the pathogenesis of DHF.21
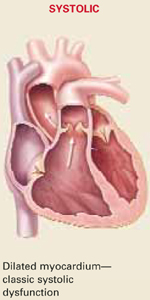
Physical examination does not help distinguish between DHF and SHF. Signs and symptoms of both disorders are relatively the same.22 Therefore, the presence of one or more of these risk factors in the setting of heart failure and preserved LV function supports the diagnosis of DHF.14-17TABLE 2 summarizes known clinical characteristics and features of SHF and DHF. All patients with systolic heart failure have some component of diastolic dysfunction as well.10,12,23,24
TABLE 2
Characteristics of patients with systolic vs diastolic heart failure
| Differentiating systolic and diastolic dysfunction | ||
| Etiology | Commonly associated with previous MI; exists concurrently with diastolic dysfunction | Pathogenesis is multifocal; associated more often with systemic hypertension, may exist alone without a component of systolic heart failure |
| Gender-specific differences | Both sexes affected | More common in women |
| Age-related differences | All ages affected | More common in elderly patients |
| Echocardiographic findings | Depressed LVEF <40% | Preserved LVEF >40% |
| Symptomatology | Identical—unable to differentiate with clinical examination | Identical—unable to differentiate with clinical examination |
| Long-term prognosis | 15% annual mortality rate | 5 to 8% annual mortality rate |
| MI, myocardial infarction; LVEF, left ventricular ejection fraction. | ||
Diagnosis is made clinically
No consensus exists on standardized criteria for diagnosing diastolic heart failure. However, 3 diagnostic levels—possible, probable, and definite DHF—have been proposed by Vasan and Levy.11
Possible DHF is defined as signs and symptoms of heart failure (TABLE 3) in patients with normal LV function, but lacking an assessment of ventricular function in proximity to the heart failure event.
Probable DHF is defined as (1) signs and symptoms of heart failure and (2) an ejection fraction >50% measured via echocardiography or radionuclide angio-graphy within 72 hours of the heart failure exacerbation.
Definite DHF is defined as (1) signs and symptoms of heart failure, (2) an ejection fraction >50% measured via the above methods within 72 hours of the patient’s presentation, and (3) increased left-ventricular end diastolic pressure (LVEDP) measured during cardiac catheterization.
TABLE 3
Modified Framingham criteria for diagnosing heart failure
| Need 2 major or 1 major and 2 minor fulfilled criteria for diagnosis of heart failure. |
|---|
| MAJOR CRITERIA |
| Paroxysmal nocturnal dyspnea |
| Orthopnea |
| Elevated jugular venous pressure |
| Pulmonary rales |
| Cardiomegaly on radiography |
| Acute pulmonary edema |
| S3 gallop |
| Weight loss >4.5 kg in response to treatment of heart failure |
| MINOR CRITERIA |
| Bilateral ankle/leg edema |
| Nocturnal cough |
| Dyspnea on ordinary exertion |
| Hepatomegaly |
| Pleural effusion |
| Tachycardia >120 bpm |
| MAJOR OR MINOR |
| Weight loss >4.5 kg in 5 days in response to treatment of heart failure |
| From: McKee et al, N Engl J Med 1971; 285:1441-1446.26 |