VAIL, COLO. – Children with congenital malformations or a variety of chronic diseases are at a previously undescribed, sharply increased risk for serious respiratory syncytial virus infection, according to a landmark Danish study.
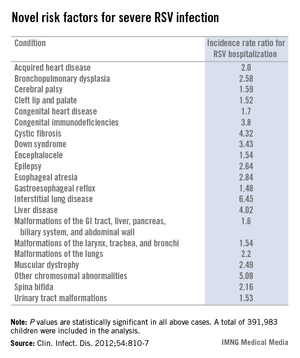
Among the newly identified risk factors for hospitalization for RSV infection are neuromuscular disease, interstitial lung disease, liver disease, congenital malformations, liver disease, and congenital immunodeficiencies, Dr. Eric A.F. Simões said at a conference on pediatric infectious diseases sponsored by the Children’s Hospital Colorado.
"When you are fighting with an insurance company over whether treatment with palivizumab is appropriate, you can show them this study. It’s the only one of its kind," said Dr. Simões, a coauthor of the Danish study and professor of pediatrics at the University of Colorado, Denver.
This was a population-based cohort study including 391,983 children born in Denmark during 1997-2003. Dr. Simões and his coinvestigators utilized the comprehensive Danish National Patient Registry to determine that 2.7% of the children carried a diagnosis for one or more chronic diseases, a broad heading which included congenital malformations, chromosomal abnormalities, and acquired chronic disorders.
During their first 23 months of life, 2.8% of the study population was hospitalized for an RSV infection. Of those hospitalized children, 8.8% had at least one diagnosis of chronic disease. In a multivariate analysis adjusted for maternal smoking, prematurity, hospitalization within the last 30 days, and other potential confounding factors, the incidence rate ratio for RSV hospitalization in children with any congenital chronic condition was 2.18. For children with any acquired chronic condition, it was 2.25. (See chart.)
Dr. Simoes and his colleagues put forth biologically plausible mechanistic explanations for the increased risks of severe RSV in many of the newly identified at-risk subgroups. For example, they argued that children with cleft lip and palate are known to have a high incidence of middle ear disease, and it’s possible that difficulties in swallowing could result in aspiration of infected nasal secretions, with resultant lower respiratory tract RSV infection.
Children with various neuromuscular diseases were found to be at increased risk for RSV hospitalization. These included children with epilepsy, cerebral palsy, muscular dystrophy, and spina bifida or other congenital malformations of the nervous system. Moreover, children with neuromuscular disease also had significantly longer-than-average RSV hospitalizations. It’s possible that the increased RSV morbidity seen in these patients was due at least in part to diminished vital capacity secondary to muscular dysfunction, coupled with disrupted clearance of respiratory secretions, the investigators speculated.
The finding of an elevated risk of RSV hospitalization among children with malformations of the urinary system might be explained as follows: Lower urinary tract obstruction results in oligohydramnios, in turn resulting in pulmonary hypoplasia.
The 4.32-fold increased risk of severe RSV infection documented in this study in children with cystic fibrosis may be related to the reduced levels of surfactant proteins A and D, which characterize this disease. Those proteins are key components of the pulmonary innate immune system, Dr. Simões and his coworkers noted (Clin. Infect. Dis. 2012;54:810-7).
In contrast, the finding of a fourfold increased risk of RSV hospitalization in children with liver disease was unexpected, and the investigators had no explanation for it.
The Danish study was supported by Abbott Laboratories. Dr. Simões has received research grants from and served as a consultant to Abbott and half a dozen other companies, as well as UNICEF, the Bill & Melinda Gates Foundation, and the World Health Organization.