Diagnosis requires careful history and exam
Community-acquired MRSA SSTIs are often diagnosed based on the patient’s history and risk factors, along with physical exam findings. Common findings include single or multiple erythematous pustules, furuncles, carbuncles, cellulitis, and abscesses. Patients may confuse the initial lesion with an insect or spider bite,12 as occurred with the patient in our opening scenario.
If purulent drainage is present, perform a swab for culture and sensitivity to confirm the diagnosis of MRSA and assist in antibiotic selection.13 If a patient with an SSTI does not respond to beta-lactam antibiotics, consider MRSA until proven otherwise.
Once confirmed by microbiological assessment, follow Centers for Disease Control and Prevention guidelines to differentiate CA-MRSA from HA-MRSA.14 It is important to distinguish between the two, as patients with HA-MRSA are at greater risk for antibiotic failure and progression to more invasive infections.
Confirmation of a CA-MRSA infection requires all of the following criteria:14
• Diagnosis was made in the outpatient setting or by positive culture within 48 hours of admission to the hospital
• No history of MRSA infection or colonization
• No history in the past year of hospitalization; admission to a skilled nursing facility or hospice; dialysis; or surgery
• No permanent indwelling catheters or medical devices that go through the skin.
Confirmation of an HA-MRSA infection requires at least one of the following criteria:14
• It occurs more than 48 hours after admission to the hospital.
• There is a prior history of MRSA infection or colonization.
• There is a history in the past year of hospitalization; admission to a skilled
nursing facility, nursing home, or hospice; dialysis; or surgery.
• The presence of any indwelling catheter or medical device that passes through the skin into the body.
Rely on evidence-based treatment protocols
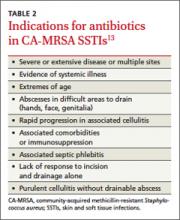
In 2011, the Infectious Disease Society of America (IDSA) published consensus guidelines for CA-MRSA to assist with evidencebased decision making. Primary treatment of cutaneous abscesses remains incision and drainage alone without antibiotics, except under certain circumstances (TABLE 2).13 The guidelines recommend antibiotic treatment with empiric coverage for CA-MRSA when purulent cellulitis exists. However, if cellulitis exists without purulence or abscess formation, antibiotic coverage for CA-MRSA is not encouraged for initial treatment.13
Empiric antibiotic coverage for uncomplicated CA-MRSA SSTIs managed in the outpatient setting should include clindamycin, trimethoprim/sulfamethoxazole (TMPSMX), a tetracycline, or linezolid for 5 to 10 days. Factors including cost, patient age and comorbidities, drug allergies, and local resistance patterns should guide the initial antibiotic you choose. TMP-SMX and tetracyclines are relatively inexpensive (<$20), clindamycin is more costly, and linezolid is often costprohibitive as standard treatment.
Do not prescribe tetracyclines for children younger than 8 years of age because of the risk of permanent tooth discoloration. Clindamycin is the only category “B” antibiotic in the group that can be used during pregnancy, and renal impairment needs to be taken into consideration with TMP-SMX and linezolid. For very minor skin lesions in children, mupirocin 2% topical ointment appears to be the therapy of choice.13
Although IDSA has not provided strong recommendations about treatment of asymptomatic close household contacts, this may be considered as another means of attempting to control the spread of MRSA in the community.
Provide patient education. Patient education is paramount to successful treatment and prevention. Explain to patients that people living in close quarters with individuals who already have the bacteria on the skin are far more likely to be carriers. Overcrowding situations that pose a risk include military installations, prisons, long-term care facilities, athletic teams, and daycare centers.
To prevent MRSA, encourage patients to wash their hands often and shower regularly, especially after exercise. Also keep cuts, scrapes, and wounds clean and covered until they heal. Avoid sharing personal items, such as towel and razors.
Finally, remind patients to get care early if they think they may be infected. Symptoms suggestive of MRSA include a red, swollen, painful area on the skin that may look like a spider bite. The area may contain pus and be accompanied by a fever.
Provide close outpatient follow-up within a few days of initiating therapy to document clinical response and aid in further decision-making. Signs of more extensive cellulitis may signal a need for a change of antibiotics or parenteral therapy. Similarly, joint or bone pain underlying areas of cellulitis, significant myalgias or muscle pain out of proportion to exam, or systemic symptoms such as fever, chills, nausea, or lethargy might indicate more extensive infection requiring inpatient treatment.