Transformation of inpatient activities. We reorganized inpatient teams to include clinician representatives from the clinics whose patients were being treated. This process ensured better continuity of experience and familiarity with the environment of care and discharge/follow-up processes for both patients and all providers.
Additionally, inpatient teams developed new workflows to ensure that all involved members of the outpatient team were well informed of the hospitalization process. On the first or second day of admission, a hospital follow-up document was electronically routed to the administrative support staff, the PCP team nurse, and the PCP (FIGURE 1). An integrated EMR created a link between the hospital and all ambulatory practices that allowed for real-time transmission of patient information. The document identified the timing of a follow-up appointment and requested a 48-hour phone call from the team nurse after hospital discharge. The inpatient team also included a concise summary of the hospitalization for the PCP, to aid in anticipating patient discharge and any impending needs. The document was retrievable and traceable in the EMR.
Study groups and statistical analysis
The Oregon Health & Science University’s Institutional Review Board (IRB#9768) determined this study was not human subjects research because the proposed activity did not meet the definition of human subject per 45 CFR 46.102(f). The board made this determination because our analysis file included only hospital readmission rates and no patient-level data.
Adult patients admitted by the inpatient teams consisted of 2 distinct populations: patients whose PCP practiced at one of the 4 outpatient clinics (Group 1 patients); and patients admitted from other, unaffiliated clinics (Group 2 patients). In contrast to the transformations in patient care described in Group 1, care provided to Group 2 patients was considered usual care, as there was no interface between outpatient and inpatient teams to revise operations. Patients in either group were excluded from analyses if they died during the hospitalization. Maternity patients were also excluded.
We identified the percentage of patients readmitted within 30 days of a hospital admission using administrative data sources, which underwent careful data checking and validation, and were sub-grouped according to whether the patients were in Group 1 or Group 2. We used group-specific and overall linear regression to examine the changes in percentage of readmission within 30 days of discharge in the 2 study groups over 12 months, including a model that specifically assessed the interaction between Group 1 readmission percentages and those in Group 2. We considered a P-value ≤.05 to be significant in this exploratory study.
RESULTS
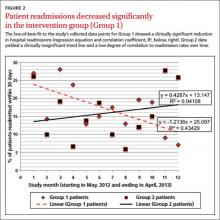
Patient readmissions decreased significantly
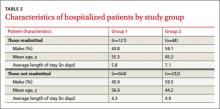
Our analysis included 961 patients; 685 patients (71.3%) were in Group 1, and 276 (28.7%) were in Group 2 (Table 2). The distribution of patient gender and mean age was similar within groups for patients readmitted and not readmitted during the study period. Among patients readmitted, the mean hospital length of stay was 5.8 days and 7.1 days for Group 1 and Group 2, respectively. Among those not readmitted, the mean hospital length of stay was 4.3 and 4.9 in Group 1 and 2, respectively.
The percentage of patients readmitted per month ranged from 28.1% to 7.1% in Group 1 and 27.8% to 5.9% in Group 2 (Figure 2). Patient readmissions in Group 1 decreased significantly from 27% in May 2012 to 7.1% in April 2013 with an R2 of 0.43 (P=.02). Readmissions of patients in Group 2 were more variable; 26.1% in May 2012 and 25.9% in April 2013 with a non-significant R2 of 0.04 (P=.53). The regression model (unadjusted) that compared the interaction between Group 1 and Group 2 readmissions over the study period was significant, indicating a decrease in readmissions in Group 1 and no strong correlation between usual care and readmissions over time in Group 2 (P=.05).
DISCUSSION
Implementing intensive coordinated care management and transition processes in a group of primary care clinics appears to significantly decrease hospital readmissions for patients in Group 1, compared with those in Group 2 who received usual care. While it is possible that some of the ambulatory practices in Group 2 admitting patients to the inpatient services were using or developing care coordination programs including hospital follow-up, none of these providers or groups interfaced with the inpatient teams in this study. We are, therefore, confident that Group 2 providers were not undertaking any new or novel activities that reached in to hospital inpatient services to improve care coordination.