SNOWMASS, COLO. – The latest heart failure guidelines from the American College of Cardiology/American Heart Association place a new emphasis on aldosterone antagonists as a central aspect of the management of symptomatic or previously symptomatic heart failure with reduced ejection fraction – while underscoring important caveats to their use.
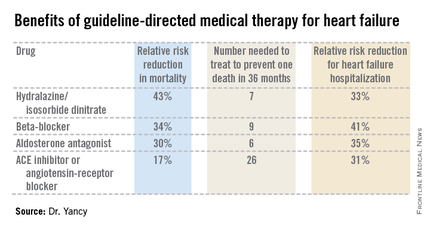
Aldosterone antagonist therapy earns the strongest possible designation in the guidelines: a Class I/Level of Evidence A recommendation. This is based on data from multiple randomized trials showing that, used appropriately, these agents result in a 30% relative risk reduction in mortality and a 35% reduction in the relative risk of heart failure hospitalization, with a number needed to treat for 36 months of just six patients to prevent one additional death. Those figures place the aldosterone antagonists on a par with the other Class I/A heart failure medications – beta-blockers, ACE inhibitors or angiotensin receptor blockers, and hydralazine/isosorbide dinitrate in African Americans – in terms of benefits (see chart).
"These data are quite striking," Dr. Clyde W. Yancy observed in presenting highlights of the 2013 ACC/AHA guidelines at the Annual Cardiovascular Conference at Snowmass.
"For many years, we’ve functioned in a space where we thought there’s not that much we can do for heart failure, and I would now argue stridently against that. You can see the incredibly low numbers needed to treat here. Only a handful of patients need to be exposed to these therapies to derive a significant benefit on mortality. These are data we should incorporate in our clinical practice without exclusion," declared Dr. Yancy, who chaired the heart failure guideline-writing committee.
The important caveat regarding the aldosterone antagonists is that they should be used only in patients with an estimated glomerular filtration rate greater than 30 mL/min per 1.73 m2 and a serum potassium level below 5.0 mEq/dL. Otherwise that Class I/A recommendation plummets to III/B, meaning the treatment is inappropriate and potentially harmful, continued Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
The guidelines emphasize the imperative to implement what has come to be termed guideline-directed medical therapy, known by the acronym GDMT. The panel found persuasive an analysis showing that heart failure patients with reduced ejection fraction who were on two of seven evidence-based, guideline-directed management interventions had an adjusted 38% reduction in 2-year mortality risk compared with those on none or one, while those on three interventions had a 62% decrease in the odds of mortality and patients on four or more had mortality reductions of about 70% (J. Am. Heart Assoc. 2012;1:16-26).
The seven interventions are beta-blockers, ACE inhibitors or ARBs, aldosterone antagonists, anticoagulation for atrial fibrillation, cardiac resynchronization therapy, implantable cardioverter-defibrillators, and heart failure education for eligible patients.
The guidelines advise strongly against the combined use of an ACE inhibitor and ARB. It’s an either/or treatment strategy. Studies indicate there is no additive benefit with the combination, only an increased risk of side effects.
An important innovation in the guidelines is the new prominence afforded to heart failure with preserved ejection fraction, known as HFpEF (pronounced heff-peff).
"What’s most different in the new heart failure guidelines is that we have uploaded HFpEF to the front page," said Dr. Yancy. "We want you to appreciate how important it is. We recognize that there’s no evidence-based intervention that changes its natural history; rather, the focus is on identification and treatment of the comorbidities. It’s important to emphasize that this is a novel way of thinking about heart failure for a very important iteration of that disease."
Among the other highlights of the guidelines is a clarification of the current role for biomarker-guided heart failure therapy. B-type natriuretic peptide (BNP) or N-terminal pro-BNP measurements are deemed useful in making the diagnosis of heart failure as well as in establishing prognosis. Serial measurements can be used to titrate GDMT to optimal doses. But there are as yet no data to show that using the biomarkers to titrate GDMT to higher doses improves mortality.
The 2013 ACC/AHA Guideline for the Management of Heart Failure was developed in collaboration with the American Academy of Family Physicians, the American College of Chest Physicians, the Heart Rhythm Society, and the International Society for Heart and Lung Transplantation (J. Am. Coll. Cardiol. 2013;62:e147-e239).
Dr. Yancy reported having no financial conflicts.