A scathing new report by the Centers for Disease Control and Prevention found ample room for improvement in inpatient antibiotic prescribing.
Findings include continued overuse of antibiotics in hospitals, errors in prescribing, and the lifesaving potential of efforts to reduce antibiotic use:
• Physicians in some hospitals prescribed three times as many antibiotics as doctors in other hospitals, even though patients were being cared for in similar areas of each hospital.
• Antibiotic prescriptions contained an error in 37% of cases involving treatment for urinary tract infections or use of the common and critical drug, vancomycin (Vancocin).
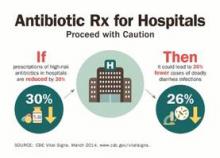
• Models predicted that a 30% decrease in the use of broad-spectrum antibiotics would lead to a 26% reduction in Clostridium difficile infections, which kill roughly 14,000 hospitalized patients each year.
"Antibiotics are often lifesaving, and we have to protect them before our medicine chests run empty," CDC director Tom Frieden said during a press conference highlighting the report, released in the CDC’s March 4 Morbidity and Mortality Weekly Report (MMWR 2014 March 4;63:1-7).
Dr. Frieden announced that the CDC’s fiscal 2015 budget, part of President Obama’s budget initiative rolled out today, contains a $30 million increase in funds to establish a robust infrastructure in the United States to detect antibiotic threats and protect patients and communities.
The new monies would allow the CDC to extend the "detect and protect" strategy to combat antibiotic resistance outlined last year, help support state and hospital efforts to implement antibiotic stewardship programs, and improve rapid detection of antimicrobial threats and outbreaks.
"One of the things that makes us so focused on antimicrobial resistance is that not only is it a really serious problem, but [also] it’s not too late," Dr. Frieden said.
If funded, he anticipates the CDC and other stakeholders will be able to reverse drug resistance and cut in half the rate of C. difficile and the "nightmare" carbapenem-resistant Enterobacteriaceae infections.
It was noted that robust efforts to improve the use of antibiotics associated with C. difficile in the United Kingdom have resulted in more than a 50% reduction in use of those targeted agents and a roughly 70% reduction in C. difficile infections over the past 6 to 7 years.
The CDC is strongly recommending that every hospital in the United States have an antibiotic stewardship program and is providing a new checklist to help facilities with the task. The checklist contains seven core elements of an effective program: leadership commitment; accountability for outcomes under a single leader; drug expertise under a single pharmacist leader; taking action on at least one prescribing improvement practice; tracking antibiotic prescribing and resistance patterns; reporting regularly to staff about these patterns; and educating staff on antibiotic resistance and improving prescribing practices.
Specific advice was also given to clinicians to order recommended cultures before antibiotics are given and to start drugs promptly; make sure the indication, dose, and expected duration are specified in the patient record; and reassess patients within 48 hours and adjust treatment, if necessary, or stop treatment, if indicated.
Concerns were raised during the briefing over whether voluntary strategies will curb interfacility transmission caused by transfers of patients with multidrug-resistant infections and the failure to report outbreaks between facilities. Dr. John R. Combes, the American Hospital Association’s senior vice president said several groups are working to smooth out these transfers and that the AHA’s "Hospitals in Pursuit of Excellence" program provides best practices to facilitate transfers and foster cooperation with surrounding facilities to prevent infections.
The new CDC report is based on a review of data from all 323 hospitals in the MarketScan Hospital Drug Database and from hospitals in the CDC’s Emerging Infections Program.
Antibiotics were prescribed for 55.7% of patients hospitalized in 2010 in the MarketScan Hospital Drug Database, with 30% receiving at least one dose of broad-spectrum antibiotics.
One or more antibiotics were used to treat active infections in 37% of 11,282 patients treated in 2011 at 183 acute care hospitals evaluated by the Emerging Infections Program. Half of the antibiotics were prescribed for one of three scenarios: lower respiratory tract infections (22.2%), urinary tract infections (14%), and suspected drug-resistant Gram-positive infections such as methicillin-resistant Staphylococcus aureus (17.6%).
The CDC previously called on physicians to address antibiotic resistance in its Antibiotic Threats in the United States, 2013 report and the 2013 Get Smart About Antibiotics Week. The issue also will be tackled in the CDC’s forthcoming Transatlantic Taskforce on Antimicrobial Resistance 2013 report, with additional research expected to focus on contributing factors that led to such wide variances in antibiotic use between hospitals.