Primary care specialties continue to gain interest from medical school seniors, according to the results of the 2014 Main Residency Match, but their interest probably isn’t great enough to keep pace with the growing physician workforce demands.
In another record-setting year, the Match offered 29,671 first- and second-year residency positions, up 500 from its previous high in 2013. More than half of the new positions were in internal medicine and family medicine, according to the National Resident Matching Program.
In internal medicine, 247 first-year residency positions were added to the Match. Family medicine offered 72 more spots, and pediatrics offered 24 more positions.
The extra positions added up to gains in the number of U.S. medical school graduates choosing residencies in internal medicine and family medicine. But fewer U.S. seniors matched to pediatrics in 2014 than in the previous year.
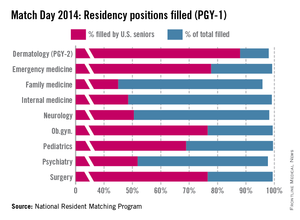
In internal medicine, 6,524 positions were offered this year. Of those, 99.1% were filled, with 48.5% taken by U.S. medical graduates.
In 2014, 3,109 family medicine residency positions were offered. Of those, 95.8% were filled, with 45% filled by U.S. medical graduates.
In pediatrics, 99.5% of the total 2,640 positions offered were filled. U.S. medical graduates filled 68.9% of the pediatric positions. Fewer (19) U.S. graduates filled pediatric positions, compared with 2013, reversing a trend of steady increases.
The take-home message from primary care leaders is that it was overall a very good year in the Match. But many more good years are needed to meet growing workforce demands stemming from the Affordable Care Act and the aging population.
"There has been growth in primary care," said Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians. "I’m just concerned that it’s not sufficient to meet the needs of the population as we go forward."
One reason for his concern is that even though more medical students are opting for internal medicine residencies, there’s no guarantee that they will become primary care physicians in the end. Only about 20% to 25% of these residents will stay in general internal medicine, while the rest will subspecialize, Dr. Alguire said.
Pediatrics faces the same situation, said Dr. Reid Blackwelder, president of the American Academy of Family Physicians, as many of the medical students choosing pediatrics on Match Day will end up subspecializing. So projecting the future workforce capacity based on the figures from the Match could lead to "overly optimistic" projections, he said.
"We’re definitely moving in the right direction," Dr. Blackwelder said. "But we really need to have an accelerated increase."
To meet the workforce needs, the AAFP estimates that family medicine residencies must add and fill 65 new positions each year through 2025. They exceeded that goal in 2014, but that trend will need to continue every year for a decade to have an effect, Dr. Blackwelder said.
One way to attract more medical students to primary care is to fix one of the critical issues for physicians in practice: declining payments. The AAFP is advocating for better pay for primary care physicians, by moving away from the current fee-for-service system, which rewards volume of services over quality and efficiency.
High student debt also continues to be a barrier to recruiting young primary care physicians, Dr. Alguire said.
"Any student with an eye to the future would have to be worried about how they’re going to pay the debt off and how quickly they can pay that debt off," he said. "And they may be beginning to wonder if the primary care field is really the answer economically."
Outside of primary care, surgical specialties continued to be popular in this year’s Match. The most competitive specialties in 2014 were neurological surgery, orthopedic surgery, otolaryngology, plastic surgery, and radiation oncology. Each of those specialties offered at least 50 positions in the Match program and filled at least 90% of the positions with U.S. medical school seniors.
The top specialties are more competitive than ever, said Mona M. Signer, executive director of the National Resident Matching Program.
"If any applicant is applying to a very competitive specialty, they need to consider what their backup plan is," she said. "Not everyone can be an orthopedic surgeon."
One surprise in this year’s Match was that fewer U.S. seniors participated. There were 89 fewer U.S. seniors registered for the Match, and 113 fewer U.S. seniors submitted rank order lists of program, Ms. Signer said.