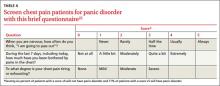
Panic disorder. Several tools have been proposed for screening for panic disorder (PD),23,24 but none have been tested in patients with chest pain. Dammen et al25 developed a 3-item questionnaire to assess for PD among patients with chest pain who were referred for cardiac evaluation (TABLE 4).25 A score ≥5 on the Dammen questionnaire had 55% sensitivity and 86% specificity for PD, with a PPV of 71% and an NPV of 76%.25 Although this instrument has not been subjected to validation studies, using it may help clarify whether further investigation for PD is warranted.
Psychotherapeutic interventions may be effective for patients whose chest pain is caused by PD. A Cochrane review of 15 randomized controlled trials of psychological interventions for chest pain in patients with normal coronary anatomy found that cognitive-behavior therapy, and possibly hypnotherapy, reduced patient reports of chest pain, reduced chest pain frequency, and increased the number of chest pain-free days, at least for 3 months.26
What to do when the diagnosis remains unclear
When your initial evaluation and diagnostic testing yield no clear diagnosis, appropriate follow-up is vital because in the year after primary care patients first develop chest pain, they are 1.5 to 3 times more likely than the general population to be diagnosed with musculoskeletal, GI, psychological, or respiratory problems, nearly 5 times as likely to be diagnosed with heart failure, and nearly 15 times as likely to be diagnosed with coronary heart disease.27,28
Consider ordering exercise or chemical stress testing within 3 to 7 days for a patient with chest pain that suggests ACS but who has normal results on EKG and biomarker testing.8 Interestingly, though, in a study of 4181 patients in an ED chest pain unit who had 2 sets of normal serum troponins during a 6-hour period followed by exercise or chemical stress testing, only 470 patients (11%) had abnormal stress test results and only 37 (.9%) had obstructive CAD that would have potentially benefited from revascularization.29 Thus, testing troponin levels twice over 6 hours is a reasonable alternative to stress testing for a primary care patient with chest pain; stress testing would be unnecessary if both troponin values were normal.
CASE › Based on her current chest pain symptoms, Ms. Z’s MHS is a reassuringly low 1, so CAD is unlikely. However, she scores 5 on the Dammen panic disorder screen. Due to her financial concerns, you decide to forgo stress testing and instead draw a serum troponin now, with plans to repeat later in the afternoon at your clinic lab if the initial result is normal. You encourage her to try a high-dose PPI for 2 weeks to determine whether GERD may be contributing to her symptoms, and offer to help her explore counseling options to address her emotional stressors.
CORRESPONDENCE
William E. Cayley Jr, MD, MDiv, University of Wisconsin, UW Health Augusta Family Medicine Clinic, 207 West Lincoln, Augusta, WI 54722; bcayley@yahoo.com