A 19-year-old male complaining of shortness of breath was transferred from our facility’s urgent care unit to our emergency department. He had a 2-week history of hemoptysis and vomiting, and over the previous week, he had developed mild hematemesis. His other symptoms included left thigh, flank, and upper quadrant pain; left chest pain exacerbated by exertion, light-headedness, and palpitations. He said that over the past 8 months, he’d been tired and lost some weight.
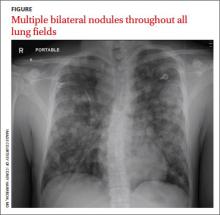
His blood pressure was 138/77 mm Hg, pulse was 142 beats per min, respiratory rate was 22 breaths per min, and oxygen saturation was 93% on room air. The physical exam revealed normal breath sounds and a diffusely tender abdomen. We ordered a chest X-ray (FIGURE).