Intensive behavioral counseling reduces risky sexual behaviors and the likelihood of sexually transmitted infections, and is recommended for all sexually active adolescents and adults who are at increased risk for acquiring or transmitting STIs, according to the U.S. Preventive Services Task Force.
In a separate but related recommendation statement, the USPSTF called for screening for chlamydia and gonorrhea in sexually active females aged 24 years or younger, and in older women at increased risk for infection.
Both recommendation statements were published online Sept. 23 in Annals of Internal Medicine.
The counseling recommendation updates a 2008 USPSTF recommendation, and is based on a review of the evidence for behavioral counseling in the primary care setting. The task force found adequate evidence in support of behavioral counseling, and concluded with moderate certainty that such counseling results in a moderate net benefit, reported Dr. Michael L. LeFevre, the task force chair and professor and associate chair of family medicine at the University of Missouri at Columbia.
The updated recommendation reaffirms the value of high-intensity behavioral counseling for those at increased risk of STIs and acknowledges that some interventions of lesser intensity are also effective.
Clinicians should be aware of populations at particularly high risk for STIs, according to the task force.
“African Americans have the highest STI prevalence of any racial/ethnic group, and STI prevalence is higher in American Indians, Alaska Natives, and Latinos than in white persons,” according to the recommendation statement (Ann. Internal. Med. 2014 Sept. 23 [doi:10.7326/M14-1965]).
Other high-risk groups include men who have sex with men, those with low incomes living in urban settings, current or former inmates, military recruits, those who exchange sex for money or drugs, those with mental illness or disability, those who use or have used drugs, those with a history of sexual abuse, and patients at public STI clinics.
Counseling interventions ranging in intensity from 30 minutes to 2 or more hours of contact time are beneficial, the task force said, noting that the evidence indicates that the benefits of counseling increase in tandem with the level of intensity.
Interventions can be delivered by primary care clinicians or by trained behavioral counselors, and the most successful approaches provide basic information about STIs and STI transmission, include risk assessment, and provide training in condom use, communication about safe sex, problem solving, and goal setting.
Interventions can include face-to-face counseling, videos, written materials, and telephone support.
The recommendation statement is based on a commissioned systematic review of the literature, which included 31 trials that reported STI outcomes and/or sexual behavioral outcomes in adolescents or adults (Ann. Internal Med. 2014 Sept. 23 [doi:10.7326/M14-0475]).
The chlamydia and gonorrhea screening recommendation statement updates a 2007 chlamydia recommendation and expands the 2005 gonorrhea recommendation to include all sexually active females aged 24 and younger. The updated statement is based on evidence that screening can accurately detect chlamydia and gonorrhea, and reduces complications of both infections with a moderate magnitude of benefit.
The review found insufficient evidence to assess the balance of benefits and harms of screening in men (Ann. Internal Med. 2014 Sept. 22 [doi:10.7326/M14-1981).
The highest infection rates occur in women aged 20-24 years, followed by those aged 15-19 years, the task force said.
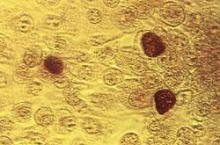
“Chlamydia trachomatis and Neisseria gonorrhoeae infections should be diagnosed via nucleic acid amplification tests because their sensitivity and specificity are high and they are approved by the Food and Drug Administration for use on urogenital sites, including male and female urine, as well as clinician-collected endocervical, vaginal, and male urethral specimens,” according to the statement.
Evidence with respect to screening intervals is lacking, and a reasonable approach would be to screen patients whose sexual history reveals new or persistent risk factors since the last negative test results, the USPSTF said, adding that posttest counseling is an integral part of managing patients who are diagnosed with an STI.
The chlamydia and gonorrhea screening recommendation also is based on a commissioned systematic review of recent literature, including 10 fair-quality studies on diagnostic accuracy, 1 good-quality randomized controlled trial of sexually active young women, and large cohort studies of screening in pregnant women at increased risk for infection.
An estimated 20 million new cases of STIs occur each year in the United States, and half of these occur in adolescents and young adults aged 15-24 years. Chlamydia and gonorrhea are the most commonly reported STIs in the United States, with more than 1.4 million cases of chlamydia and more than 330,000 cases of gonorrhea reported in 2012, according to the USPSTF, which stated that these new recommendations are important because many STIs are asymptomatic and can result in serious sequelae such as pelvic inflammatory disease, infertility, and cancer.