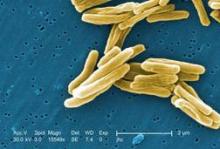
Three different short-course treatment regimens for tuberculosis failed to show noninferiority to the standard 6-month course in separate phase III randomized clinical trials, even though the experimental regimens produced a more rapid decline in bacterial load, as expected, according to reports published online Oct. 23 in the New England Journal of Medicine.
The main reason that the short-course (4-month) approaches failed to measure up to standard treatment was that, despite their greater bactericidal activity, the rate of relapse was excessive after treatment was completed.
Researchers undertook these large international trials because the data from several phase II and murine studies had been so promising: replacing either the isoniazid or the ethambutol in the standard anti-TB regimen with a fluoroquinolone appeared to permit shortening of the treatment period without sacrificing efficacy. But the consistently negative results from these phase III studies clearly demonstrate that this approach is not effective.
The first trial involved 1,931 adults with newly diagnosed and untreated Mycobacterium tuberculosis infection who were treated in South Africa, India, Tanzania, Kenya, Thailand, Malaysia, Zambia, China, and Mexico. These patients were randomly assigned to receive the standard regimen of isoniazid, rifampin, pyrazinamide, and ethambutol for 8 weeks, followed by 18 weeks of isoniazid plus rifampin (control group, 640 participants); or an experimental regimen in which ethambutol was replaced by moxifloxacin for 17 weeks, followed by 9 weeks of placebo (655 participants); or an experimental regimen in which isoniazid was replaced by moxifloxacin in the same way (636 participants), said Dr. Stephen H. Gillespie of the University of St. Andrews (England) and University College London and his associates.
Patients in the two experimental groups converted to culture-negative status more rapidly than did those in the control group. However, in a per-protocol analysis, 92% of the control group achieved a favorable final outcome, compared with only 85% and 80% of the experimental groups, respectively. Results of a modified intention-to-treat analysis and of more than 20 sensitivity analyses showed the same pattern. At the end of active treatment, only 12 patients in the control group had a relapse of TB infection, compared with 64 patients and 46 patients, respectively, in the experimental groups, Dr. Gillespie and his colleagues said (N. Engl. J. Med. 2014 Oct. 23 [doi:10.1056/NEJMoa1407426]).
The second trial was an open-label noninferiority study involving 1,836 patients in Benin, Guinea, Kenya, Senegal, and South Africa. They were randomly assigned to standard 6-month treatment (919 control subjects) or an experimental treatment in which gatifloxacin was substituted for ethambutol and the course of therapy was shortened to 4 months (917 patients), said Dr. Corinne S. Merle of the London School of Hygiene and Tropical Medicine and her associates.