Identification of geographic clusters in which children have higher rates of underimmunization, or whose parents outright refuse vaccination, can help identify similar pockets of vaccine underutilization and help health care providers better focus their approach to providing immunization interventions around the country, according to the findings of a new study published in Pediatrics.
“For optimal public health and patient care, clinicians and health care systems ideally should tailor care to their communities,” wrote Dr. Tracy A. Lieu of Kaiser Permanente Northern California, Oakland, and her associates.
“The ability to identify clusters of underimmunization and vaccine refusal would help providers focus their efforts on the parents in communities with the greatest concerns, as well as identify areas at elevated risk for outbreaks of vaccine-preventable diseases” (Pediatrics 2015 [doi:10.1542/peds.2014-2715]).
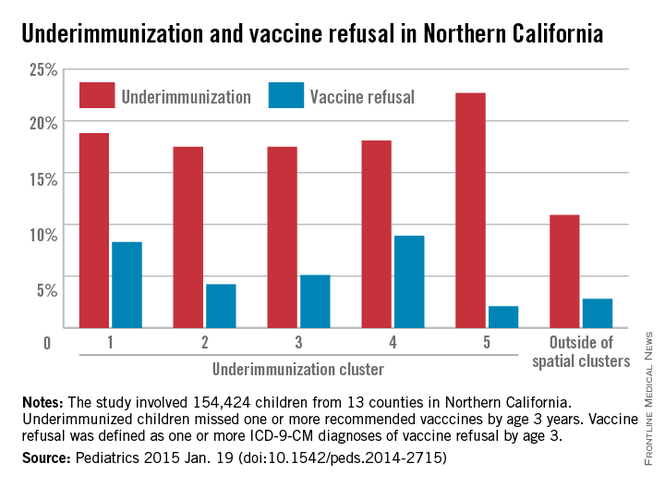
In a retrospective cohort study, Dr. Lieu and her coinvestigators looked at children with continuous membership in the Kaiser Permanente Northern California, aged from birth to age 36 months, between Jan. 1, 2000, and December 31, 2009. A total of 154,424 children in 13 northern California counties were selected for inclusion in the study. Children were classified as underimmunized if they missed at least one vaccine by age 36 months, while vaccine refusal was classified using ICD-9-CM codes V6405, V6406, or V6407, as per the International Classification of Diseases, Ninth Revision, Clinical Modification for subjects who refused even one vaccination at any time prior to age 36 months.
Spatial scan analysis of all the accumulated data revealed five statistically significant geographic clusters in which underimmunization was more pronounced, nearly all located in the greater Sacramento and San Francisco metropolitan areas, with underimmunization rates over the course of the study period ranging from 18.1% in northern San Francisco and southern Marin counties to 22.7% in Vallejo (P = .023 and P = .042, respectively).