High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
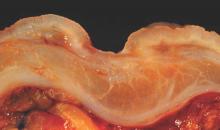
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.