Midostaurin completely resolved at least one type of organ damage for 45% of patients with advanced systemic mastocytosis, based on a multicenter, open-label, phase II, industry-sponsored trial.
“Response rates were similar regardless of the subtype of advanced systemic mastocytosis, KIT mutation status, or exposure to previous therapy,” reported Jason R. Gotlib, MD, of Stanford (Calif.) University, and his associates. Adverse effects led to dose reductions for 41% of patients, however, and caused 22% of patients to stop treatment, the researchers wrote online June 29 in the New England Journal of Medicine.
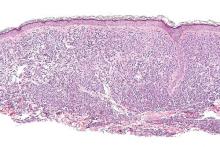
Systemic mastocytosis is related to a constitutively activated receptor tyrosine kinase encoded by the KIT D816V mutation. As neoplastic mast cells infiltrate and damage organs, patients develop cytopenias, hypoalbuminemia, osteolytic bone lesions, abnormal liver function, ascites, and weight loss. Mastocytosis lacks effective treatments, and patients with aggressive disease tend to live about 3.5 years, the researchers noted (N Engl J Med. 2016 Jun 29;374:2530-40).
Of 116 patients with advanced systemic mastocytosis, 27 lacked measurable signs of disease or had unrelated signs and symptoms. The remaining 89 patients included 16 with aggressive systemic disease, 57 with systemic disease and an associated hematologic neoplasm, and 16 with mast cell leukemia. Patients received 100 mg oral midostaurin twice daily in continuous 4-week cycles for a median of 11.4 months, with a median follow-up of 26 months.
In all, 53 (60%) patients experienced at least 50% improvement in one type of organ damage or improvement in more than one type of organ damage, said the researchers. These responders included 12 patients with aggressive systemic mastocytosis, 33 patients with systemic mastocytosis and a hematologic neoplasm, and eight patients with mast-cell leukemia. No one achieved complete remission, but after six treatment cycles, 45% of patients had complete resolution of at least one type of organ damage.
Patients typically experienced, at best, a nearly 60% drop in bone marrow mast cell burden and serum tryptase. The median duration of response was 24 months, median overall survival was 28.7 months, and median progression-free survival was 14.1 months. Mast cell leukemia and a history of treatment for mastocytosis were tied to shorter survival, while a 50% decrease in mast cell burden significantly improved survival (hazard ratio, 0.33; P = .01).
Grade 3 or 4 hematologic abnormalities included neutropenia (24% of patients), anemia (41%), and thrombocytopenia (29%). Marked myelosuppression was associated with baseline cytopenia and may have reflected either treatment-related effects or disease progression, the researchers said. The most common grade 3/4 nonhematologic adverse effects were fatigue (9% of patients) and diarrhea (8%).
Novartis Pharmaceuticals sponsored the study, and designed it and collected the data with the authors. Dr. Gotlib disclosed travel reimbursement from Novartis. Ten coinvestigators disclosed financial ties to Novartis and to several other pharmaceutical companies. Two coinvestigators disclosed direct research support from Novartis. The remaining four coinvestigators had no disclosures.