Scientists have found evidence to suggest that a genetic alteration in osteoblasts can induce acute myeloid leukemia (AML).
And this provides a potential therapeutic target for AML and myelodysplastic syndromes (MDS).
Stavroula Kousteni, PhD, of Columbia University Medical Center in New York, and her colleagues described these findings in Nature.
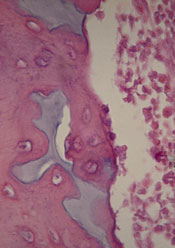
The researchers discovered that an activating mutation of beta-catenin in mouse osteoblasts induces AML.
This mutation leads to cancer in adjacent hematopoietic stem cells (HSCs) through a series of events. First, the mutated beta-catenin protein moves from its normal location on the exterior of the osteoblast to the cell’s nucleus, where it activates production of the protein jagged1.
Jagged1 proteins are then shipped to the osteoblast’s exterior membrane, where they can bind to Notch proteins—which activate signaling pathways—on neighboring HSCs. When this happens, Notch transmits signals inside the HSCs that enable leukemic transformation.
To confirm the role of jagged1 in AML development, the investigators removed 1 allele of jagged1 in osteoblasts. This decreased Notch signaling in Lin-Sca+c-Kit+ cells, rescued anemia and deregulation of HSC lineage differentiation, and prevented AML development.
The researchers then evaluated the effects of blocking Notch signaling using a gamma-secretase inhibitor. The treatment reversed hematopoietic deregulation and myeloid expansion in the blood, marrow, and spleens of the mice and reversed their AML.
“If the [process] works the same way in humans, our study suggests practical ways that we may be able to intervene with a drug or an antibody,” Dr Kousteni said.
With this in mind, she and her colleagues analyzed cells from 107 patients with AML or MDS. About 38% of the patients had changes in beta-catenin, jagged1, and Notch signaling that mirrored the changes in the mice. But none of the 56 healthy control subjects studied had these changes.
The investigators therefore concluded that these findings provide new insight into AML/MDS pathogenesis and may have implications for treatment.

