Individuals with HIV have a sixfold greater likelihood of also being infected with hepatitis C virus, according to a global systematic review and meta-analysis published in Lancet Infectious Diseases.
Researchers analyzed 783 studies of the prevalence of HIV and hepatitis C virus (HCV) infection, providing co-infection estimates for 88 countries, and found the odds of HCV infection among individuals with HIV was 5.8 times higher than in HIV-negative individuals, with an overall co-infection prevalence of 6.2% in HIV-infected individuals.
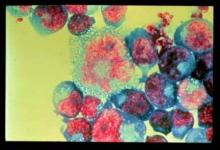
“People living with HIV without treatment are less likely to spontaneously clear HCV infection, have higher HCV viral loads, and experience more rapid HCV disease progression than those without HIV infection,” wrote Lucy Platt, Ph.D., from the London School of Hygiene & Tropical Medicine, and her coauthors.
The co-infection prevalence was lower in general population samples (2.4%) and pregnant or heterosexually exposed samples (4%), but slightly higher in men who have sex with men (6.4%) and significantly higher among individuals who inject drugs (82.4%).
The highest prevalence of co-infection in general population samples was in North Africa and the Middle East, while the highest prevalence of co-infection among men who have sex with men was found in North America, and the highest prevalence of co-infection among pregnant women was in western and central Africa (Lancet Infect Dis. 2016 Feb 24. doi: 10.1016/S1473-3099(15)00485-5).
The study was funded by the World Health Organization. One author declared funding from the Medical Research Council UK and membership in the STOP-HCV Consortium.