DISCUSSION
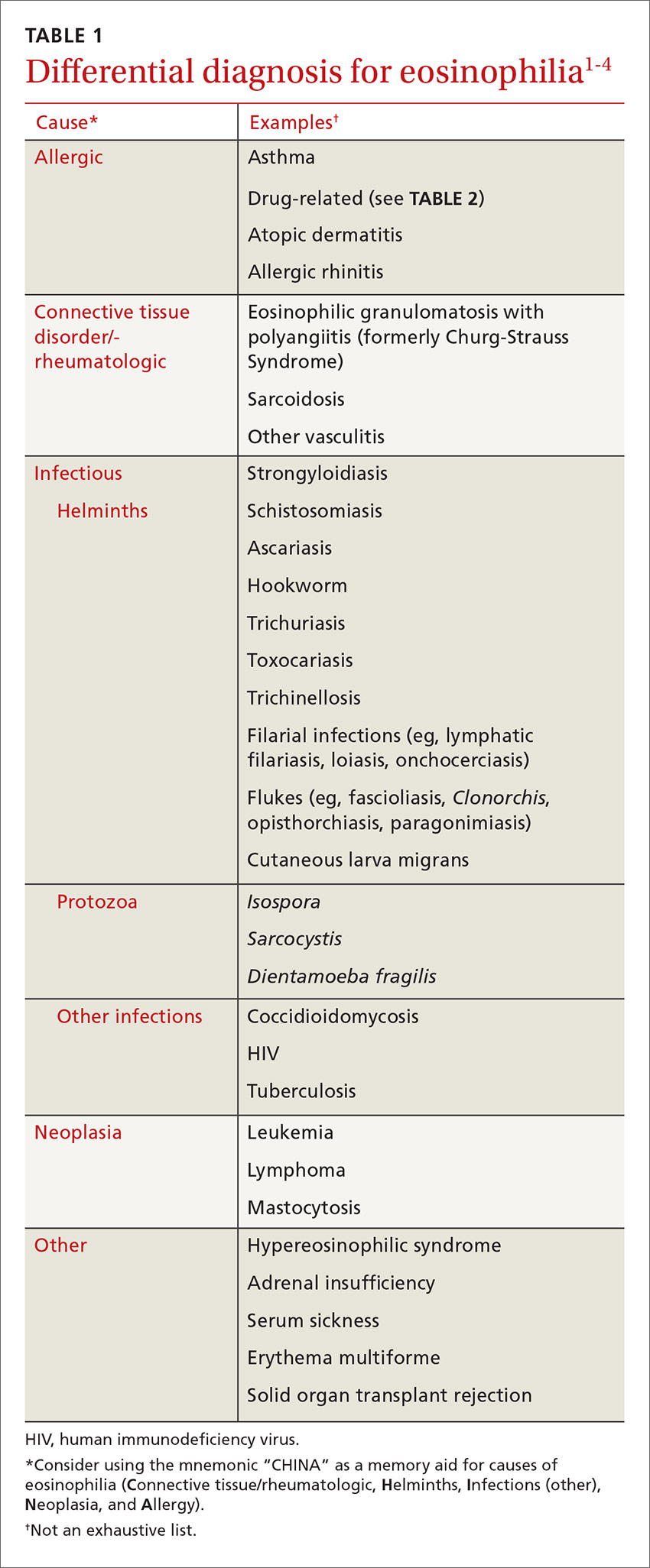
These 2 cases highlight how the presentation of eosinophilia can vary and how important it is to maintain a broad differential diagnosis (TABLE 11-4). Causes of eosinophilia are numerous and can be divided into 3 categories: primary, secondary, and idiopathic.1,5 Hematologic malignancy, where eosinophilia is clonal, is an example of a primary etiology. Causes of secondary eosinophilia include infectious diseases, drugs (TABLE 25), autoimmune disorders, and allergic conditions. Prolonged eosinophilia that is >3 x 109/L is associated with end-organ damage. Dermatologic, pulmonary, gastrointestinal, and cardiac involvement is most common.2
Eosinophilia associated with parasitic infection
In returning travelers and international adoptees, multicellular helminthic parasites are the most common causes of eosinophilia, with eosinophilia occurring during tissue migration or penetration.1,3
Strongyloides stercoralis is found in tropical and temperate areas. Its life cycle involves both a parasitic and free-living component. It has the ability to autoinfect the host and can cause hyperinfection in those who are immunocompromised. Acute infection is often subclinical, but may include a skin rash or nonspecific intestinal symptoms.1 Patients commonly present with asymptomatic eosinophilia. Diagnosis is most often via serology, and the first-line treatment for uncomplicated cases is ivermectin 200 µg/kg/day orally for 2 days.4