THE CASE
A 44-year-old woman with a 15-year history of type 2 diabetes sought care for a firm, non-tender mass in the medial lower quadrant of her right breast. She hadn’t experienced any skin changes or axillary lymphadenopathy. The patient had immigrated to California from Afghanistan 22 years earlier, at which time she was briefly married to an Afghan man suffering from a chronic cough.
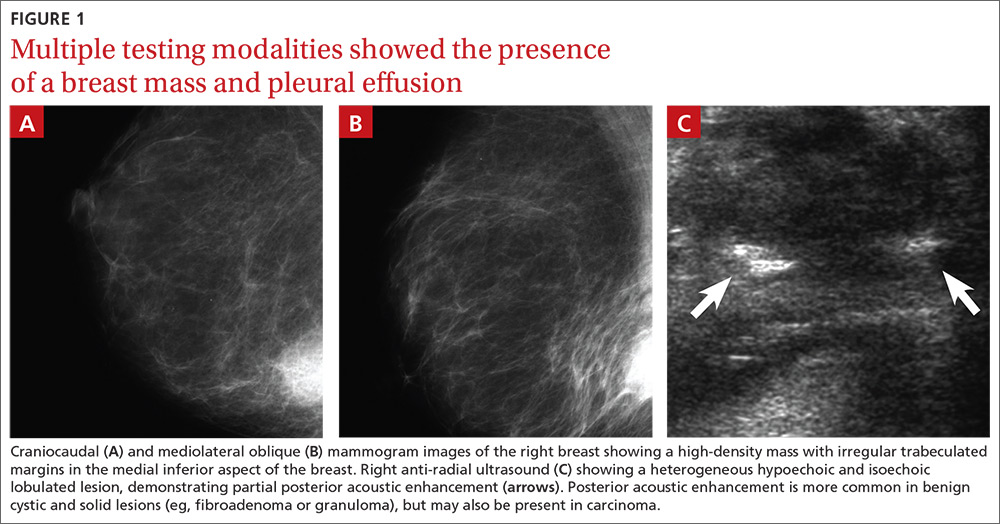
Mammography revealed a 3.5 x 4 x 4 cm lesion at the chest wall, which was highly suspicious for carcinoma (FIGURES 1A AND 1B). Sonography showed a heterogenous hypoechoic and isoechoic mass with posterior acoustic enhancement (FIGURE 1C). An excisional biopsy was performed.
One week postoperatively, the patient presented to the emergency department for a worsening nonproductive cough that intensified when supine, and was associated with subscapular pleuritic pain. She denied fever or weight loss. Biopsy results were pending.
THE DIAGNOSIS
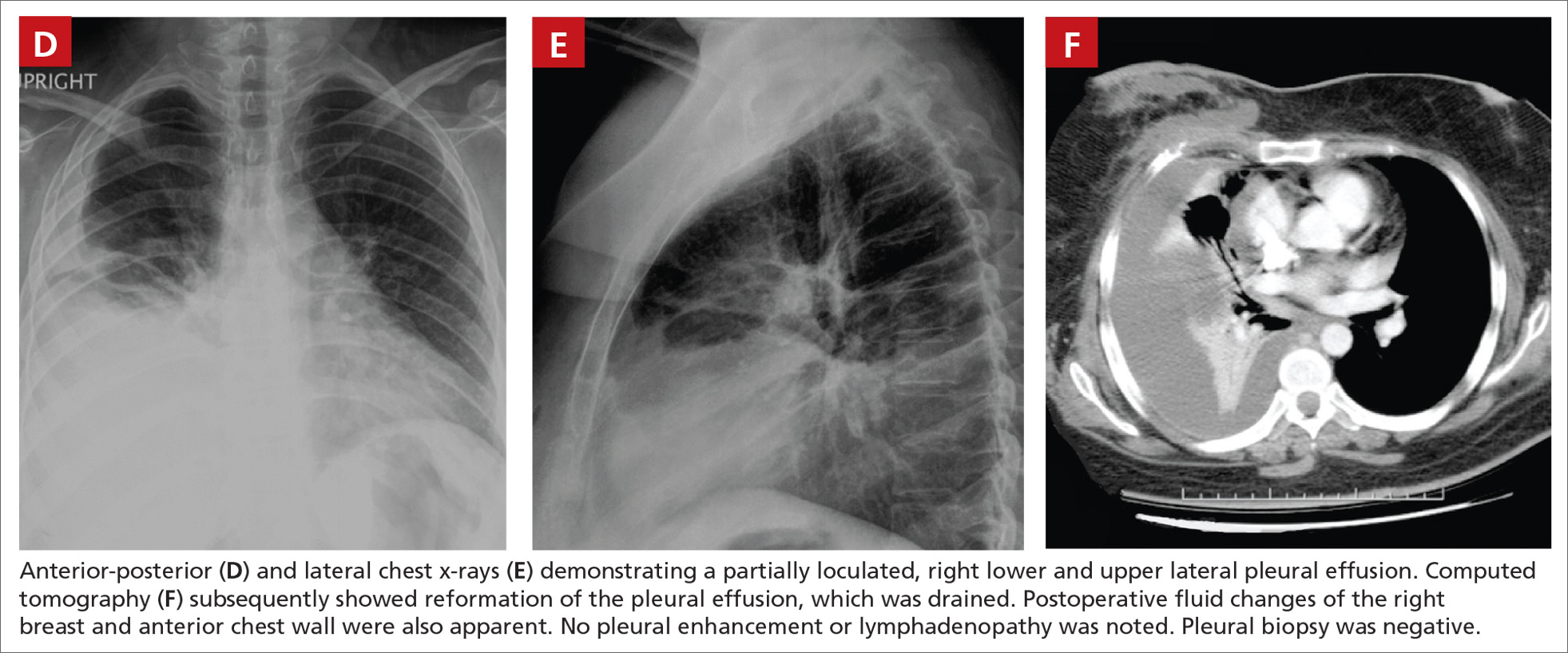
Chest x-rays revealed a large right pleural effusion that was presumed to be malignant (FIGURES 1D AND 1E). Thoracentesis yielded 1.5 liters of tea-colored exudate containing 2800 nucleated cells/mL—63% lymphocytes and 37% neutrophils—and a pleural fluid to serum protein ratio >0.5. Adenosine deaminase was <1 U/L. Fluid Gram stain, acid-fast bacillus (AFB) fluorescent antibody testing, AFB cultures, and cytology were negative. Computed tomography (CT) subsequently demonstrated recurrent effusion without hilar or mediastinal lymphadenopathy or pleural enhancement (FIGURE 1F).
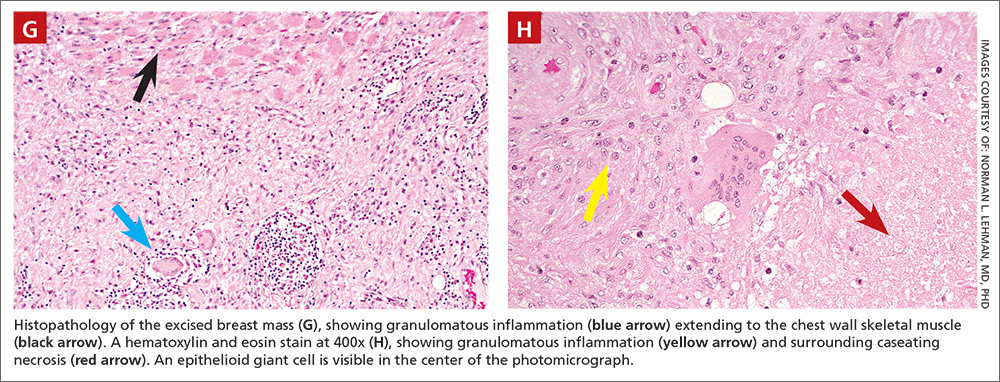
Histologically, the breast mass showed caseating granulomatous inflammation (FIGURES 1G AND 1H). An AFB stain was negative. Polymerase chain reaction (PCR) performed on DNA extracted from the formalin-fixed, paraffin-embedded biopsy material was positive for Mycobacterium tuberculosis.1 A CT-guided pleural biopsy showed only normal tissue. A follow-up tuberculin skin test (purified protein derivative [PPD]) yielded a 10-mm indurated reaction.