THE CASE
A 41-year-old, right-hand dominant man sought care at our facility one day after trying to pull his boat out of the water. He’d tried to lift the boat with his hands while his forearms were fully supinated and his elbows were flexed to about 90°. He then felt a sharp burning sensation in his left anterior shoulder and was unable to lift the boat. The patient denied feeling a popping sensation at the time of the injury. He had mild pain at night, but was able to sleep. He said that he had mild diminished strength with elbow flexion, but denied having any numbness, tingling, or discoloration of his skin.
The patient said he did weightlifting and strength training of his upper and lower extremities 4 times/week. He was in good general health, was not taking any medications or supplements, and denied smoking or using illicit drugs. His surgical history was significant for a Bankart repair 8 years ago.
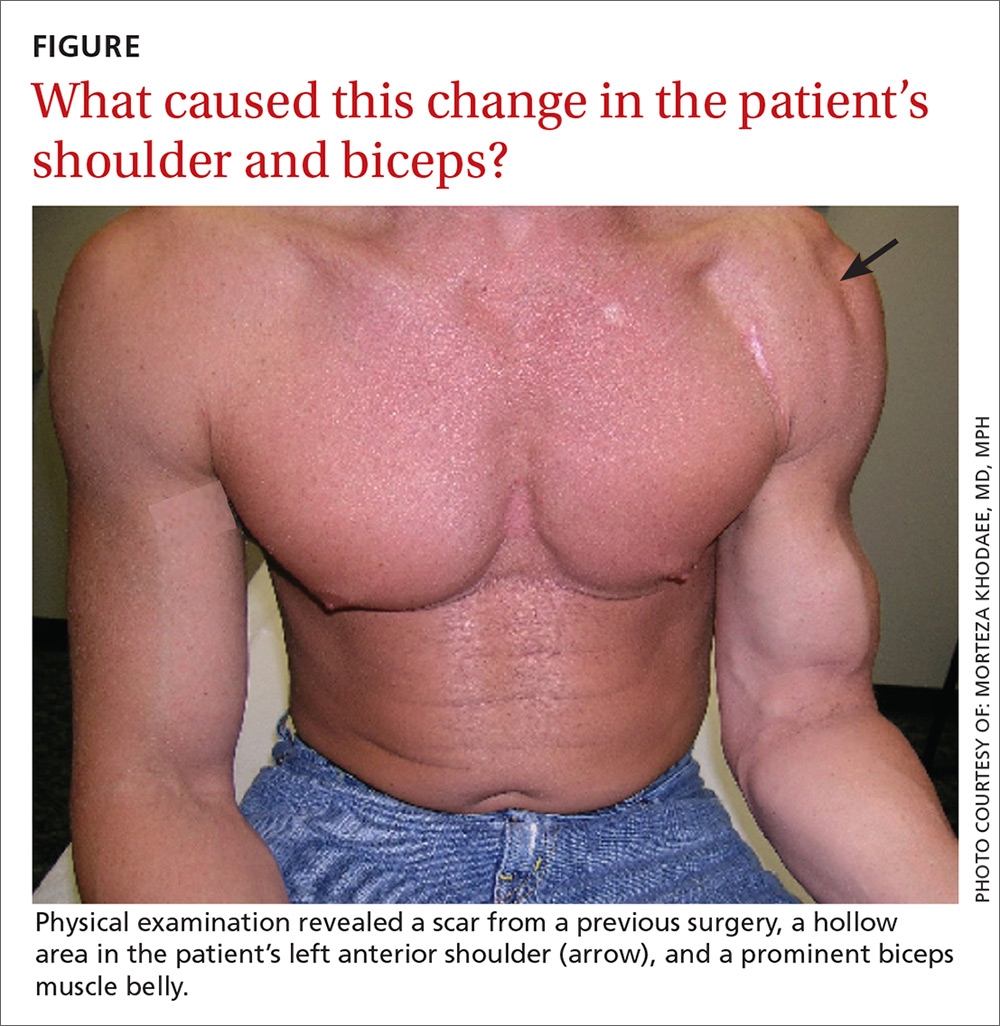
On physical examination, the patient had a scar from the previous surgery, a hollow area in his left anterior shoulder, and a prominent biceps muscle belly (FIGURE). His shoulder range of motion was normal. Left shoulder Neer, Hawkins-Kennedy, drop-arm, cross-arm, empty can, and apprehension tests were negative. A left Speed’s test (resisted elbow flexion when elbow is flexed 20° to 30° with the forearm in supination and the arm in about 60° of flexion) was positive for mild anterior shoulder pain. So, too, was a Yergason’s test (resisted forearm supination and elbow flexion when forearm is pronated and elbow is flexed to 90°). The patient’s elbow flexion strength was 4 out of 5, and his supination strength was 5 out of 5. Neurovascular and sensory examinations of his upper extremities, including radial and ulnar pulses, were normal.
THE DIAGNOSIS
A diagnostic musculoskeletal ultrasound revealed an empty tendon sheath of the long head of the biceps in the bicipital groove and a retracted echogenic stump with associated hematoma at the proximal musculotendinous junction. Based on the patient’s history, physical examination, and ultrasound, a diagnosis of an acute rupture of the left long head of the biceps brachii tendon was made.
DISCUSSION
Diagnosis of acute rupture is often made clinically based on a visually apparent defect proximally and a bulbous mass distally (“Popeye deformity”).1 Ultrasound and magnetic resonance imaging (MRI) may aid in the diagnosis by demonstrating an absence of the long head in the bicipital groove or at its insertion.
The biceps brachii tendon functions in flexion and supination of the forearm. The long head of the biceps also plays a stabilizing role in the glenohumeral joint during elbow flexion and supination.2 Injury to the biceps most often occurs in middle-aged men following a traumatic sudden eccentric bicipital contraction event, during which most patients describe a snapping or popping sensation.3,4
Rupture of the proximal biceps tendon represents about 90% of all biceps ruptures, which almost exclusively involve the long head of the biceps.3,5,6 Risk factors for tendon rupture include obesity, smoking, steroid injection in or around the tendon, and previous tendinopathy.7-10
Functional limitations. It is generally thought that functional limitations following a proximal biceps rupture are relatively minimal, due to the work of other flexors and supinators, including the brachialis and brachioradialis. However, because strength and endurance of the muscle can decrease by about 25%, physical laborers and high-demand athletes may notice a degree of residual weakness with supination and elbow flexion.11,12