A 44-year-old African-American woman with sickle cell trait presented to the clinic to establish care. She complained of polyarthralgias that she’d had since adolescence; the pain was worst in her right shoulder. She reported morning stiffness that lasted up to 8 hours, an intermittent facial rash, oral ulcers, joint edema (of which she had pictures on her phone), and photosensitivity. She took ibuprofen and acetaminophen as needed for pain. She once worked as a medical assistant but hadn’t been able to work since 2014 due to pain. She reported having been told as a teenager that she might have juvenile arthritis, but she didn’t recall ever having diagnostic tests performed or receiving treatment other than anti-inflammatories.
A couple of weeks after an initial visit with a rheumatologist, the patient returned to the family medicine clinic. She said she was upset that the specialist had x-rayed her hands, but had not checked her shoulder, which was the primary source of her pain. She also had pain in her hands, hips, feet, and knees.
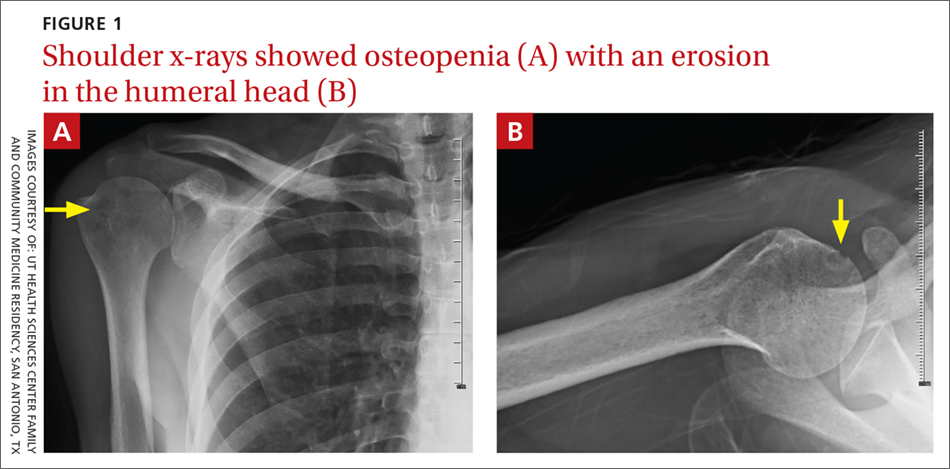
On physical exam, the patient looked fatigued. A musculoskeletal exam revealed no joint effusions or edema, but was significant for right shoulder pain with reduced abduction to 90°. Gross motor strength was 5/5 in all 4 extremities. Laboratory testing revealed an antinuclear antibody titer of 1:160 and was negative for double-stranded DNA. Bilateral hand and foot x-rays showed no joint erosions. An x-ray of the right shoulder was obtained, which showed evidence of osteopenia and an erosion in the humeral head (FIGURES 1A and 1B).