The genetic basis of MRKH syndrome is unknown. These patients have normal female karyotypes and phenotypes with normal ovaries and ovarian function—although there is evidence that they are prone to early menopause. They develop secondary sexual characteristics. They usually present with primary amenorrhea at 15 to 17 years of age.
Vaginal agenesis is the second most common cause of primary amenorrhea after gonadal dysgenesis. Most patients have a rudimentary, nonfunctioning uterus, but 2% to 7% have a uterus with functioning endometrium and present with cyclic or chronic abdominopelvic pain secondary to obstruction or endometriosis, hematocolpos, or hematometra.
Imaging. US examination facilitates evaluation of the kidneys and confirms the presence of ovaries and absence of the uterus. MRI may be useful to confirm the presence of functioning endometrium.
The differential diagnosis of vaginal agenesis includes androgen insensitivity and low-lying transverse vaginal septum. Treatment includes psychosocial support to reassure the patient that a normal sex life will be possible after treatment.5 Construction of a neovagina, using vaginal dilators (the first-line strategy) or surgical placement of split-thickness skin graft or artificial skin (Abbe–McIndoe procedure), is the treatment. In one case series, more than 90% of patients with vaginal agenesis were successfully treated using vaginal dilation.6
The American College of Obstetricians and Gynecologists (ACOG) recommends that patients be referred to centers with expertise in surgical creation of a neovagina.5
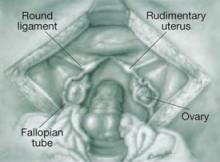
FIGURE 5 Uterine agenesis
This depiction of uterine agenesis shows small, nonfunctioning müllerian remnants and normal tubes and ovaries.
Agenesis of the lower vagina
This malformation is caused by a failure of canalization of the sinovaginal bulbs and vaginal plate. The tubes, ovaries, cervix, and upper vagina are normal, but the lower vagina is replaced by fibrous tissue. Adolescents present with primary amenorrhea accompanied by cyclic pelvic pain. A vaginal dimple may be apparent on external inspection.
Because these girls have normal cyclic pituitary–ovarian–endometrial function at menarche, the upper vagina will distend with blood and secretions, and a mass can be palpated on rectoabdominal examination. US confirms the presence of a fluid-filled mass, and MRI further defines the length of obstruction.
Treatment. Surgery (by an experienced vaginal surgeon) is best performed when a large hematocolpos is present because distention increases the amount of tissue available for pull-through.
CASE 3 Fusion failure
A 17-year-old woman complains of lower abdominal pain and an enlarging abdomen. Menarche occurred at 13 years. The patient began to notice right-sided lower abdominal pain and abdominal swelling about 2 years ago, but denies any other symptoms.
Examination reveals a mass arising from the right lateral vaginal wall. The cervix appears to be normal. US shows a large, predominantly right-sided, fluid-filled mass arising from the pelvis. The uterus appears to be didelphic, with normal ovaries and an absent right kidney.
What is the mass?
This is a classic description of uterovaginal duplication that arises when the müllerian ducts fail to fuse (FIGURE 6).
In this case, the right-sided vagina failed to canalize as well, causing a large hematocolpos. Generally, duplication is limited to the uterus and cervix (uterus didelphys bicollis), although duplication of the vulva, bladder, urethra, vagina, and anus have been described.
Women with a didelphic uterus often have a good reproductive outcome. A septated vagina occurs in 75% of cases and may cause difficulty with sexual intercourse or vaginal delivery. Symptomatic women usually opt for resection of the vaginal septum.
Women who have an obstructed hemivagina and ipsilateral renal agenesis have regular menses because menstrual blood from one uterus can exit through its unobstructed side.
Treatment involves resection of the wall of the obstructed vagina, creating a single vaginal vault. If both vaginas have failed to canalize, the patient will present much earlier, with primary amenorrhea and cyclic pelvic pain—a presentation similar to that of transverse septum. Reconstructive surgery of the uterus is not recommended for complete duplication of the uterus.1,7
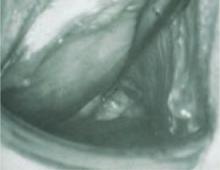
FIGURE 6 Uterus didelphys
This patient has uterus didelphys with an obstructed hemivagina.
Unicornuate and bicornuate uterus
A unicornuate uterus represents an asymmetric lateral fusion defect. One cavity is usually normal, with a fallopian tube and cervix, but the failed müllerian duct can have various configurations. The affected müllerian duct may fail to develop, or it may develop partially as a horn on the uterus or a separate structure that may or may not communicate with the uterus.
Most rudimentary horns are asymptomatic, but others contain functional endometrium that is shed cyclically. If the rudimentary horn is obstructed, as is usually the case, the woman develops cyclic or chronic abdominopelvic pain that necessitates surgical excision of the horn. Endometriosis, a result of reflux, is common.