When researchers compared women who had polyps with those who had none, they found no significant differences in age, body mass index, blood pressure, gynecologic symptoms, menopausal status, use of hormone therapy, or use of the levonorgestrel-releasing intrauterine device (Mirena). Women who had endometrial polyps scored significantly higher, however, than women who did not on the visual analog scale for periodic bleeding and on the Pictorial Blood Assessment Chart—even when women who had myomas were excluded from the analysis. Although mean hemoglobin levels were similar between groups, women who had polyps had a significantly lower mean ferritin level (25 μg/L vs 41 μg/L; P = .05).
Polyps that persisted were larger from the start
Polyps regressed spontaneously in eight women, six of whom had the feeding vessel visualized at the initial consultation. Polyps that persisted after 12 months were significantly larger (mean polyp length, 15.1 mm; SD, 5.3 mm; 95% CI, 12.7–17.5) at study inception than were those that regressed (mean polyp length, 10.7 mm; SD, 3.9 mm; 95% CI, 7.5–14.0). Polyps that persisted beyond 1 year became significantly longer during follow-up, increasing from a mean length of 15.1 mm to 18.1 mm (SD, 7.9 mm; 95% CI, 0.7–5.3; P = .01).
Twenty of the 22 women who had persistent polyps underwent transcervical resection, one underwent laparoscopic supracervical hysterectomy, and one refused treatment. There were no complications.
Histology revealed that the polyps were benign in 16 women (80%), polypoid in two women (10%), and myomas in two women (10%). No atypical or malignant changes were observed in the polypectomy patients or among all participants.
A small, separate series (three patients) found all polyps to be 5 mm to 8 mm in length at detection, with a regression rate of 100% over several months.5
When an endometrial polyp 10.7 mm in length or shorter is detected incidentally in an asymptomatic, premenopausal woman, it is appropriate to follow it for regression, growth, or the development of symptoms rather than remove it immediately.
What variables signal a greater risk of malignancy?
Baiocchi G, Manci N, Pazzaglia M, et al. Malignancy in endometrial polyps: a 12-year experience. Am J Obstet Gynecol. 2009;201(5):462.e1–e4.
Gregoriou O, Konidaris S, Vrachnis N, et al. Clinical parameters linked with malignancy in endometrial polyps. Climacteric. 2009;12(5):454–458.
Wang JH, Zhao J, Lin J. Opportunities and risk factors for premalignant and malignant transformation of endometrial polyps: management strategies. J Minim Invasive Gynecol. 2010;17(1):53–58.
These three studies explore various aspects of a fundamental challenge: how to discriminate between polyps likely to undergo malignant transformation and those that will not.
The answer: Look for menopausal status, abnormal uterine bleeding, diabetes, obesity, and hypertension. Polyps larger than 1 cm also appear more likely to become malignant.
Details of the trials
In a retrospective study involving 1,242 women who had endometrial polyps, Baiocchi and colleagues identified 95.2% of the polyps as benign, 1.3% as premalignant, and 3.5% as malignant. Four clinical variables were significantly associated with premalignant and malignant features:
- age
- menopausal status
- abnormal uterine bleeding
- hypertension.
In their series of 516 cases, Gregoriou and associates found 96.9% of polyps to be benign, 1.2% to be premalignant, and 1.9% to be malignant. Four variables were associated with premalignant and malignant features:
- age above 60 years
- menopausal status
- obesity
- diabetes.
And in a study involving 766 patients, Wang and colleagues found 96.2% of polyps to be benign, 3.26% to involve hyperplasia with atypia, and 0.52% to be malignant. Among the variables associated with premalignant and malignant polyps were:
- polyp diameter larger than 1 cm
- menopausal status
- abnormal uterine bleeding.
When endometrial polyps are identified, the following characteristics indicate an increased risk of malignancy: age above 60 years, menopausal status, abnormal uterine bleeding, obesity, hypertension, and diabetes. Polyps larger than 1 cm are also more likely to be premalignant or malignant in nature. When any of these conditions is present, polypectomy and histology are recommended.
When a patient complains of abnormal uterine bleeding, evaluation often begins with transvaginal ultrasonography (US). Among the challenges of assessing the endometrium using US is the unreliability of endometrial thickness as a predictor of pathology. For example, Breitkopf and colleagues found that transvaginal US missed intracavitary lesions in one of six premenopausal women who had abnormal bleeding and an endometrial stripe thinner than 5 mm, for a sensitivity of 74%.6
In a separate study, Marello and colleagues used the combination of hysteroscopy and directed biopsy—the gold standard of diagnosis—to evaluate 212 postmenopausal women who had an endometrial thickness of 4 mm or less.7 (This parameter has been suggested as a cutoff for symptomatic postmenopausal women.8) Of these 212 women, 10% were found to have histologically confirmed intracavitary pathology (16 polyps and 4 submucous myomas).7 Among 13 symptomatic women in this study, three (23%) were found to have an endometrial polyp.7
These studies suggest that endometrial thickness alone should not be used to exclude benign endometrial pathology in symptomatic women, be they premenopausal or postmenopausal. No data back routine US to measure endometrial thickness in asymptomatic postmenopausal women.
Hysteroscopy and SIS are preferred
Both hysteroscopy and saline infusion sonography (SIS) have significantly better sensitivity and specificity in the diagnosis of intracavitary pathology than transvaginal US alone in women who have abnormal bleeding (FIGURE 1; VIDEOS 1, 2, AND 3 related to this article in the OBG Management Video Library at obgmanagement.com).1,9 Hysteroscopy and SIS detect polyps with equal accuracy.10 However, hysteroscopy allows for removal of endometrial polyps and directed biopsy at the time of diagnosis.9
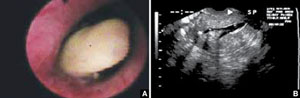
FIGURE 1 Imaging of polyps: go beyond transvaginal ultrasonography for optimal visualization
A. Hysteroscopic view of an endometrial polyp. B. The view with saline-infusion sonography.
In symptomatic women, resect the polyp
Polypectomy improves abnormal bleeding, according to a systematic review by Nathani and associates.11 All studies included in the review, which involved follow-up intervals between 2 and 52 months, reported such an improvement.11
When it is performed in the office, polypectomy offers several advantages over its inpatient counterpart:
- higher cost-effectiveness
- greater convenience
- avoidance of general anesthesia.
In both settings, it can be performed using mechanical or bipolar electrosurgical instrumentation (VIDEO 4).12
Segmental resection of the polyp while it is partially attached to the uterine wall is the optimal removal technique for large polyps (FIGURE 2). A grasping forceps can then be used to remove the polyp completely (VIDEO 5). Instruments such as a basket and snare are helpful in removing the polyp effectively.13

FIGURE 2 segmental resection of a polyp
During hysteroscopic polypectomy, the polyp is resected in segments while it is still partially attached to the endometrial wall.


