In patients with treatment-resistant schizophrenia, lithium and anticonvulsants have become such common adjuncts to antipsychotics that 50% of inpatients may be receiving them.1 Evidence supporting this practice is mixed:
- Initial case reports and open-label studies that showed benefit have not always been followed by randomized clinical trials.
- Lack of clear benefit also has been described (Table 1).
This article examines the extent of this prescribing pattern, its evidence base, and mechanisms of action that may help explain why some adjunctive mood stabilizers are more effective than others for treatment-resistant schizophrenia.
EXTENT OF USE
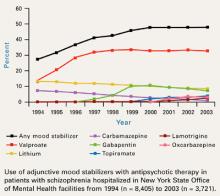
For 5 years, the rate at which inpatients with schizophrenia received adjunctive mood stabilizers has held steady at approximately 50% in New York State Office of Mental Health (NYSOMH) facilities (Figure1). These facilities provide intermediate and long-term care for the seriously, persistently mentally ill. Adjunctive mood stabilizers might not be used as often for outpatients or for inpatients treated in short-stay facilities.
Table 1
Evidence for adjunctive use of lithium or anticonvulsants for treating schizophrenia
| Agent | Case reports and open studies | Randomized, double-blind trials | Benefit? |
|---|---|---|---|
| Lithium | Yes (many) | Yes (several, +/-) | Probably not |
| Carbamazepine | Yes (many) | Yes (several; small total sample) | Limited |
| Valproate | Yes (many) | Yes | Yes |
| Gabapentin | Yes (very few, +/-) | None | Probably not |
| Lamotrigine | Yes (few, +/-) | Yes (2, +) | Yes |
| Topiramate | Yes (very few, +/-) | Yes (1, +/-) | Probably not |
| Oxcarbazepine | Yes (very few, +/-) | None | Probably not |
| + = positive results | |||
| - = negative results | |||
| +/- = both positive and negative results | |||
Valproate is the most commonly used anticonvulsant, with one out of three patients with schizophrenia receiving it. Adjunctive gabapentin use is declining, probably because of inadequate efficacy—as will be discussed later. Use of adjunctive lamotrigine is expected to increase as more data become available on its usefulness in treatment-resistant schizophrenia.
Clinicians are using substantial dosages of adjunctive mood stabilizers. During first-quarter 2004, average daily dosages for 4,788 NYSOMH patients (80% with schizophrenia or schizoaffective disorder) receiving antipsychotics were:
- valproate, 1639 mg (n = 1921)
- gabapentin, 1524 mg (n = 303)
- oxcarbazepine, 1226 mg (n = 201)
- carbamazepine, 908 mg (n = 112)
- lithium, 894 mg (n = 715)
- topiramate, 234 mg (n = 269)
- lamotrigine, 204 mg (n = 231).2
Mood-stabilizer combinations were also used. Approximately one-half of patients receiving adjunctive mood stabilizers—with the exception of valproate—were receiving more than one. In patients receiving valproate, the rate of mood-stabilizer co-prescribing was about 25%.2
WHAT IS THE EVIDENCE?
Evidence supporting the use of adjunctive lithium or anticonvulsants to treat schizophrenia varies in quality and quantity (Table 1). Case reports and open studies offer the weakest evidence but can spur double-blind, randomized clinical trials (RCTs). Unfortunately, RCTs are not often done, and the published studies usually suffer from methodologic flaws such as:
- inadequate number of subjects (insufficient statistical power to detect differences)
- lack of control of confounds such as mood symptoms (seen when studies include patients with schizoaffective disorder)
- inadequate duration
- inappropriate target populations (patients with acute exacerbations of schizophrenia instead of persistent symptoms in treatment-resistant schizophrenia).
Because controlled trials of the use of adjunctive mood stabilizers are relatively scarce, clinical practice has transcended clinical research. Clinicians need effective regimens for treatment-resistant schizophrenia, and mood-stabilizer augmentation helps some patients.
Lithium is perhaps the best-known mood stabilizer. Although early studies showed adjunctive lithium useful in treating schizophrenia, later and better-designed trials did not. The authors of a recent meta-analysis of randomized clinical trials (n = 611 in 20 studies) concluded that despite some evidence supporting the efficacy of lithium augmentation, overall results were inconclusive. A large trial would be required to detect a small benefit in patients with schizophrenia who lack affective symptoms.3
Carbamazepine use among patients with schizophrenia is declining, primarily because this drug induces its own metabolism and can require frequent dose adjustments. Adjunctive carbamazepine has been used to manage persistent aggressive behavior in patients with schizophrenia and schizoaffective disorder. Evidence comes primarily from small trials or case reports (Table 2),4-8 but results of a larger clinical trial (n = 162) by Okuma et al6 are also available
In the Okuma report—a double-blind, placebo-controlled trial of carbamazepine in patients with DSM-III schizophrenia or schizoaffective disorder—carbamazepine did not significantly improve patients’ total Brief Psychiatric Rating Scale (BPRS) scores. Compared with placebo, however, some benefit with carbamazepine did emerge in measures of suspiciousness, uncooperativeness, and excitement.
A systematic review and meta-analysis (n = 283 in 10 studies) detected a trend toward reduced psychopathology with carbamazepine augmentation for schizophrenia. BPRS scores declined by 20% and 35% in the six trials (n = 147) for which data were available (P = 0.08 and 0.09, respectively).9 Because the double-blind trial by Okuma et al6 was not randomized, it was not included in this meta-analysis.9
Figure 1 10-year trend in use of adjunctive mood stabilizers for schizophrenia
Valproate. Among the anticonvulsants, the greatest body of evidence supports the use of valproate in patients with schizophrenia,10 although a recent meta-analysis (n = 378 in 5 studies) indicates inconsistent beneficial effects.11