Optimal management of carotid stenosis to prevent death and strokes is a work in progress right now, with experts groping for the right balance between carotid endarterectomy, carotid artery stenting, and best medical therapy.
The field is bereft of both conclusive, up-to-date data and – more importantly – wide agreement on data interpretation that clearly tips treatment toward one of these options, so much so that in late January an expert panel organized by the Centers for Medicare and Medicaid Services found itself unable to support with high confidence the application of these treatments to any subgroup of carotid disease patients.
Amid this confusion are the following certainties:
- The use of carotid artery stenting (CAS) on U.S. patients grew substantially since its introduction in the late 1990s and since it began receiving limited Medicare coverage in 2004. Data collected through 2007 showed a greater-than-fourfold increase in CAS use among Medicare beneficiaries, compared with 1998 (Circ. Cardiovasc. Qual. Outcomes 2010;3:15-24).
- Other findings documented a shift in CAS use during the 2000s toward patients with asymptomatic carotid stenosis, with a recent estimate that 70%-90% of CAS patients now fall into that category (Arch. Int. Med. 2010;170:1225-7).
- The main results of the landmark CREST (Carotid Revascularization Endarterectomy vs. Stenting) trial, first reported 2 years ago (N. Engl. J. Med. 2010;363:11-23), appeared on the surface to show very similar safety and efficacy for CAS and carotid endarterectomy (CEA), but some experts caution that deeper drilling into the results show that this is an oversimplification of how the two treatments compare.
- And many experts agree that best medical therapy has improved in recent years, to the point where it deserves a new appraisal in a large trial that would compare it against carotid revascularization with CAS or CEA in asymptomatic patients. The leaders of CREST themselves have designed a new trial, CREST II, aimed at making this comparison, and have begun to vigorously lobby the National Institutes of Health to support this study.
In the meantime, vascular surgeons, endovascularists, cardiologists, and the other types of physicians who treat patients with carotid disease try as best they can to strike the right balance in how they apply the three management options.
CREST Provides New Guidance
One surgeon who has perhaps given the most thought to sorting out treatment options is Dr. Brajesh K. Lal, a co–principal investigator on CREST, a vascular surgeon at the University of Maryland in Baltimore, and a researcher who spent the past couple of years sorting through CREST’s voluminous data to find new clues to guide patient triage.
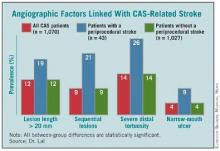
A major, recent guide for matching patients with a specific carotid intervention came from his painstaking analysis of carotid angiograms from 1,070 of the CREST patients who underwent CAS, of whom 43 patients (4%) then went on to have a stroke.
This effort identified the following four anatomical features that appear to mark patients with an increased rate of periprocedural stroke when they are treated with CAS:
- Stenotic lesion more than 20 mm long. The researchers measured lesion length as the distance from the proximal to distal shoulder of the lesion.
- Sequential lesions. This refers to two lesions separated by at least 10 mm of normal vessel.
- Severe distal tortuosity. This was defined as at least two arterial bends of at least 90 degrees that are distal to the lesion.
- Narrow-mouth ulcers. This refers to a small crater or lumen flap that produces a discrete area of contrast extension beyond the normal arterial lumen with a narrow inlet into the ulceration.
Patients with one or more of these carotid anatomical features "should be treated by endarterectomy," Dr. Lal said in an interview. "If I see any one of these in my clinical practice, I will not stent."
The variables assessed in this analysis did not include arterial calcification, as the angiographic imaging routinely collected in the study did not allow calcium quantification, said Dr. Lal. Among the stented patients in the study, the cumulative prevalence of the four significant risk markers was 39%. Patients with none of the four markers had a significantly reduced rate of periprocedural stroke during carotid stenting.
Endovascularists were already routinely assessing carotid anatomy before attempting CAS, but prior to Dr. Lal’s report on these new findings at the International Stroke Conference in New Orleans in February, "I’m not so sure that everyone has been using this [anatomical] information," he said. "When we talk about operator experience in stenting, if we don’t have the facts about what increases the stenting risk, then we won’t improve performance. You’d be surprised at what some interventionalists are willing to do," despite a patient’s challenging carotid anatomy. "These data show that you can work around a single 90-degree bend [of the distal carotid artery], but not around two bends. That is the kind of stuff we’re beginning to find out."