Case Reports

Drs. Steinbrink and Miceli are from the Department of Internal Medicine, University of Michigan Medical School, Ann Arbor. Dr. Miceli also is from the Division of Infectious Diseases. Drs. Alexis, Angulo-Thompson, Ramesh, and Alangaden are from the Department of Internal Medicine, Henry Ford Health System, Detroit, Michigan. Drs. Alexis, Ramesh, and Alangaden also are from the Infectious Diseases Section.
The authors report no conflict of interest.
Correspondence: Marisa H. Miceli, MD, Division of Infectious Diseases, University of Michigan Medical School, 1500 E Medical Center Dr, University Hospital F4005, Ann Arbor, MI 48109-5378 (mmiceli@med.umich.edu).

We identified 5 patients who had cutaneous lesions with cultures that yielded Mycobacterium marinum. It was discovered that all 5 patients had a home aquarium, and infection was preceded by trauma to the hand. However, the association between the development of the infection and exposure of the trauma site to the aquarium was not initially established until repeated questioning was performed. Skin biopsies or incision and drainage were performed for all patients, and the diagnosis was established by culture of the specimens. The mean time from initial presentation to diagnosis and initiation of appropriate treatment was 91 days (range, 21–245 days). Prolonged therapy for 2 to 6 months was necessary for resolution of the infection.
Practice Points
An environmental pathogen, Mycobacterium marinum can cause cutaneous infection when traumatized skin is exposed to fresh, brackish, or salt water. Fishing, aquarium cleaning, and aquatic recreational activities are risk factors for infection.1,2 Diagnosis often is delayed and is made several weeks or even months after initial symptoms appear.3 Due to the protracted clinical course, patients may not recall the initial exposure, contributing to the delay in diagnosis and initiation of appropriate treatment. It is not uncommon for patients with M marinum infection to be initially treated with antibiotics or antifungal drugs.
We present a review of 5 patients who were diagnosed with M marinum infection at our institution between January 2003 and March 2013.
This study was conducted at Henry Ford Hospital, a 900-bed tertiary care center in Detroit, Michigan. Patients who had cultures positive for M marinum between January 2003 and March 2013 were identified using the institution’s laboratory database. Medical records were reviewed, and relevant demographic, epidemiologic, and clinical data, including initial clinical presentation, alternative diagnoses, time between initial presentation and definitive diagnosis, and specific treatment, were recorded.
We identified 5 patients who were diagnosed with culture-confirmed M marinum skin infections during the study period: 3 men and 2 women aged 43 to 72 years (Table 1). Two patients had diabetes mellitus and 1 had hepatitis C virus. None had classic immunosuppression. On repeated questioning after the diagnosis was established, all 5 patients reported that they kept a home aquarium, and all recalled mild trauma to the hand prior to the onset of symptoms; however, none of the patients initially linked the minor skin injury to the subsequent infection.
All 5 patients initially presented with erythema and swelling at the site of the injury, which evolved into inflammatory nodules that progressed proximally up to the arm despite empiric treatment with antibiotics active against streptococci and staphylococci (Figures 1 and 2). Three patients also received empiric antifungal therapy due to suspicion of sporotrichosis.

Figure 1. A 57-year-old woman (patient 4) presented with a 6-week history of a worsening erythematous swollen painful left thumb (A). She recalled some minor trauma while cleaning her basement. One week later she noticed swelling, erythema and purulent material under the nail bed. Two weeks later she noticed an erythematous nonpainful nodule on the radial aspect of the left wrist (B), followed by the appearance of multiple tender erythematous nodules on the left forearm that followed a linear progression from the dorsal aspect of the left hand, extending over the medial aspect of the forearm and arm (C).
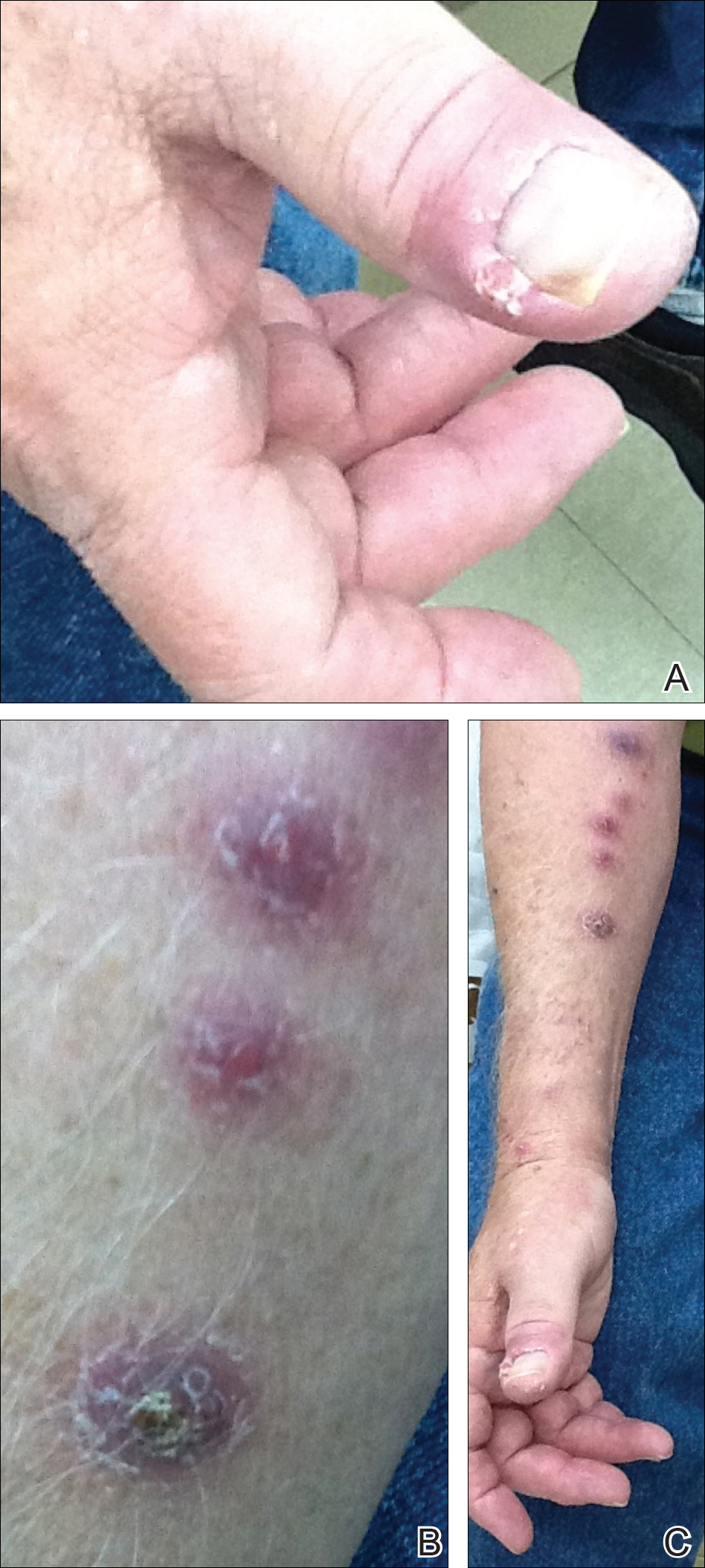
Figure 2. A 72-year-old man (patient 5) presented with pain and erythema of the right thumb after clipping the nail (A). Erythema progressed to the axilla. He was treated with bacitracin ointment and cefadroxil with no improvement. Nodular lesions developed in a linear pattern that extended to the antecubital fossa (B and C).
Skin biopsies were performed on 4 patients, and incision and drainage of purulent material was performed on the fifth patient. Histopathologic examination revealed granulomatous inflammation in 3 patients. Stains for acid-fast bacilli were positive in all 5 patients. Definitive diagnosis of the organism was confirmed by growth of M marinum within 11 to 40 days from the tissue in 4 patients and purulent material in the fifth patient. Susceptibility testing was performed on only 1 of the 5 isolates and showed that the organism was susceptible to amikacin, clarithromycin, doxycycline, ethambutol, rifampin, and trimethoprim-sulfamethoxazole (TMP-SMX).
The mean time from initial presentation to initiation of appropriate therapy for M marinum infection was 91 days (range, 21–245 days). Several different treatment regimens were used. All patients received either doxycycline or minocycline with or without a macrolide. Two also received other agents (TMP-SMX or ethambutol). Treatment duration varied from 2 to 6 months in 4 patients, and all 4 had complete resolution of the lesions; 1 patient was lost to follow-up.


Injuries from sea urchin spines are commonly seen in coastal regions with high levels of participation in water activities. Although these...

Nontuberculous mycobacteria infection is a rare sequela of hematologic malignancy, seen in only 1.5% of patients. Mycobacterium kansasii is a slow...
