High-resolution glutamate-based neuroimaging could help identify epileptic foci in individuals with epilepsy who have been assessed as nonlesional via conventional brain MRI, a study has found.
Researchers used glutamate chemical exchange saturation transfer imaging (GluCEST) in four patients with drug-resistant epilepsy who did not show lesions on MRI, and in 11 healthy controls, according to a paper published in Science Translational Medicine.
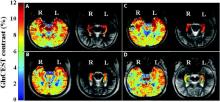
The glutamate-based imaging showed higher concentrations of glutamate in the ipsilateral hippocampus than in the contralateral hippocampus, and two independent, blinded epilepsy specialists both accurately lateralized the seizure onset in all four patients (Sci Transl Med. 2015 Oct 14. doi: 10.1126/scitranslmed.aaa7095).
Patients with drug-resistant epilepsy currently undergo a range of presurgical imaging, including 3-T MRI and single-photon emission computed tomography (SPECT), but in many patients this still fails to identify a seizure focus, despite the fact that 87% of patients in this group have previously been found to have abnormal histopathology.
“Because it is also well established that patients with lesional epilepsy have better surgical outcomes than those with nonlesional epilepsy, new neuroimaging techniques capable of detecting subtle lesions could potentially improve patient care and increase the chance of seizure freedom after surgery,” wrote Dr. Kathryn Adamiak Davis of Penn Epilepsy Center at the Hospital of the University of Pennsylvania, Philadelphia, and her coauthors.
The National Institutes of Health and the University of Pennsylvania supported the study. There were no conflicts of interest declared.