In discussion of pregnancy prevention, a great deal of time is spent on female birth control, and the use of condoms is like a tag line “Oh! And, of course, use a condom.” But are we really educating our teens on condoms, their proper use, and their prevention of sexually transmitted infections (STIs). Condoms are our basic entry level birth control, but despite their relative ease of use and accessibility, their use is on the decline.
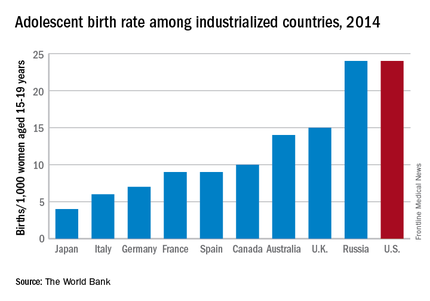
When we evaluate unintended pregnancies among teens, it is down almost 20% since 1981, according to data from the Guttmacher Institute, but compared with other developed nations, our rates are high.
In 2013, the AAP published a statement encouraging schools and pediatricians to discuss and make condoms more accessible. Fifty-four studies were done on early education of condom use, and reported a 48% increase in their use and a 42% delay in the initiation of sexual activity by 6 months.1 Despite these positive findings , condom use is still declining.
Many factors that affect their use are lack of formal education, availability, and the perception that they decrease sexual pleasure. Condom manufacturers have started campaigns that promote the image of escalating sexual pleasure, but they are competing with the media and music industry, which inundate teens with all kinds of sexual images. In review of the media, 77% showed sexual content, compared with 14% that showed risk and responsible sexual activity.
Before educating teens about condoms, we first must educate ourselves. Condoms are available in three forms: latex (80%), lamb’s cecum (15%), and synthetic (5%). Latex is considered the most effective condom in protecting against STIs and birth control. Synthetic is a good alternative to latex when a latex allergy is present, but is more prone to breakage and slippage. Lamb’s cecum prevents spread of some STIs, but because of its porous nature it does not provide protection against viruses such as HIV, hepatitis B, and herpes simplex virus (HSV). Nonlatex has a longer shelf life and is more compatible with lubricants.
Spermicide-coated condoms have fallen out of favor because the spermicide shortens the shelf life of the condom, as well as can cause mucosal irritation. When the mucosa is irritated, there is an associated increase of contracting STIs, particularly HIV.2
Make patients are aware that condoms do expire and that it is important to check the expiration date. Educating patients on the proper technique of putting a condom on is likely an awkward conversation for most, so consider directing them to the website Bedsiders.org, which has great explanations on how to use and put condoms on, along with comparisons of all types of birth control and which one is best for them.
Making condoms easily accessible is the most-important intervention. Studies show that when condoms are readily available, their use increases. The AAP advocates for schools and primary care doctors to hand them out freely.
Education is key in increasing usage of condoms and reducing spread of STIs. Encouraging parents to talk with their teen and provide access to condoms is crucial in lowering STI statistics. Although abstinence is the only 100% proof of protection, proper use of contraception is an alternative.
References
1. “Condom Use by Adolescents,” Pediatrics. 2013 Nov. doi: 10.1542/peds.2013-2821
2. “Contraception for Adolescents,” Pediatrics. 2014 Oct 10;134:e1244-56.
Dr. Pearce is a pediatrician in Frankfort, Ill. Email her at pdnews@frontlinemedcom.com.