Focus on the elbow. Whenever you suspect cubital tunnel syndrome, pay special attention to the elbow. Examine the carrying angle of the elbow in relation to the contralateral extremity. Deformity may provide clues to a history of trauma. Assess the ulnar nerve during active flexion and extension to identify a subluxatable nerve at the cubital tunnel. Examine the ulno-humeral joint for crepitus, and palpate the joint line for large osteophytes and/or ganglion cysts.
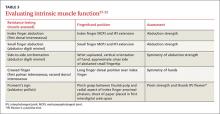
Motor examination of the ulnar nerve primarily focuses on the intrinsic muscles detailed in TABLE 3,27-32 although the flexor carpi ulnaris (FCU) and flexor digitorum profundus (FDP) to the ring finger and small finger are also innervated by the ulnar nerve. The FCU mediates the power grip, and can be tested by resisted wrist flexion and ulnar deviation. Ring finger and small finger FDP strength should be examined by resistance testing at the distal IPJ.
Provocative testing of cubital tunnel syndrome includes Tinel’s sign (performed over the cubital tunnel), the elbow flexion test (performed with elbow in maximum flexion and wrist at neutral position and held for 60 seconds), and the pressure provocation test (performed by applying pressure to the ulnar nerve just proximal to the cubital tunnel with your index and long fingers for 60 seconds while the patient’s elbow is at 20° flexion with the forearm supinated). For each test, eliciting distal paresthesia in ulnar nerve territory is a positive result. The sensitivity of these tests ranges from 70% (Tinel’s sign) to 98% (combined elbow flexion and pressure); specificity ranges from 95% to 99%.35
The scratch collapse test for cubital tunnel syndrome evaluation is similar to the version used to assess for CTS; the only difference is the location of the site that is scratched, in this case the cubital tunnel. The reported sensitivity and specificity are 69% and 99%, respectively.11
Wartenberg’s syndrome
When a patient reports paresthesia or pain along the radial aspect of the forearm that radiates into the dorsal thumb and index and middle fingers, consider Wartenberg’s syndrome—compression of the superficial radial nerve. The condition, also known as “cheiralgia paresthetica,” may exist anywhere along the course of the nerve in the forearm,36 but the compression typically occurs 9 cm proximal to the radial styloid.
Assess the skin over the forearm and hand for evidence of prior trauma, surgical scars, or external compression sources, such as a watch.37-39 Then use palpation to identify superficial or deep masses along the nerve.40 Perform Tinel’s sign by lightly tapping along the nerve course from proximal to distal in the forearm. The test is positive if paresthesias are provoked distally.41,42
Motor function of the extremity is unaffected in Wartenberg’s syndrome, unless a prior traumatic injury occurred or a comorbidity exists. Comorbidities to consider include de Quervain’s tenosynovitis, cervical radiculopathy, injury to the lateral antebrachial cutaneous nerve, and CTS.
Gross sensory testing usually is negative, but 2-point discrimination may show diminished responses. Testing distribution includes the dorsal radial wrist and hand, dorsal thumb skin proximal to the IPJ, and the dorsal surface of the index, middle, and radial half of the ring finger proximal to the IPJ.