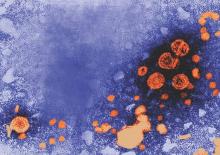
Maternal antibodies against hepatitis blunt the immune response to the hepatitis B vaccine in newborns, but the booster dose is unaffected by maternal antibodies, a study found.
Previous research also has identified a suppressed response to vaccination due to maternal antibodies with vaccines such as the measles, hepatitis A, mumps and tetanus vaccines.
“Maternal antibodies are a double-edged sword for infants,” wrote X. Chen of the Zhongnan Hospital of Wuhan (China) University, and colleagues (J Viral Hepat. 2016 Jul 29. doi: 10.1111/jvh.12572). “These neutralizing antibodies can protect neonates against most infectious diseases in early life; however, as shown in the study here, these antibodies can also suppress the immune response of infants to vaccines.”
The researchers first assessed transplacental transfer of antibodies by measuring anti–hepatitis B antibodies in 90 mothers and their newborns. The mothers were all positive for anti–hepatitis B antibodies with a median titer of 250. Before the infants had been vaccinated, 97% were positive for anti–hepatitis B antibodies. Among infants whose mothers had titers above 100 IU/L, 100% were positive for antibodies.
Then the researchers measured titers and rate of anti–hepatitis B positivity in 1,055 mothers and their 1,063 infants, aged 7-24 months, after the babies had received doses of the 10 mcg HBV vaccine at ages 0, 1 and 6 months, per the recommended schedule in China. In the United States, infants are recommended to receive the vaccine at birth, at 1-4 months, and then at 6-18 months.
Among the 405 mothers with antibodies of less than 10 IU/L, 89% of their newborns responded sufficiently to the vaccine to be positive for anti–hepatitis B antibodies. Among the 451 mothers with antibodies from 10-499 IU/L, 85% of the infants had positivity, and among the 207 mothers with antibodies of 500 IU/L and higher, 77% of the infants were positive for anti–hepatitis B antibodies.
Titers followed the same inverse pattern. The median titer was 169 in infants whose mothers had low titers, but the median titer was 79 in infants of mothers with high titers. When mothers with titers in the middle range, the infants’ median titer was 141.
Among 162 newborns who tested negative for anti–hepatitis B antibodies after receiving all three doses of the vaccine, 92% showed positivity for the antibodies after receiving a “catch-up” booster dose, without significant interference from maternal antibodies. Of another 11 infants still lacking positivity, 8 assessed 1 month later, achieved it after a second catch-up booster, suggesting “the suppression effects of the maternal anti-HBVs can be overcome.”
The research was funded by the Hongkong Zeshan Foundation, and the authors reported having no disclosures.