If organic causes are ruled out, focus on a psychiatric assessment:9
- history of the present illness (onset, symptoms, frequency, predisposing/precipitating factors)
- psychiatric history
- history of substance use
- family history of psychiatric disorders (especially anxiety disorders)
- social history (life events, including those preceding onset of panic; history of child abuse)
- medications
- mental status examination
- safety (panic disorder is associated with higher risk of suicidal ideation).
TREATMENT INCLUDES CBT AND MEDICATION
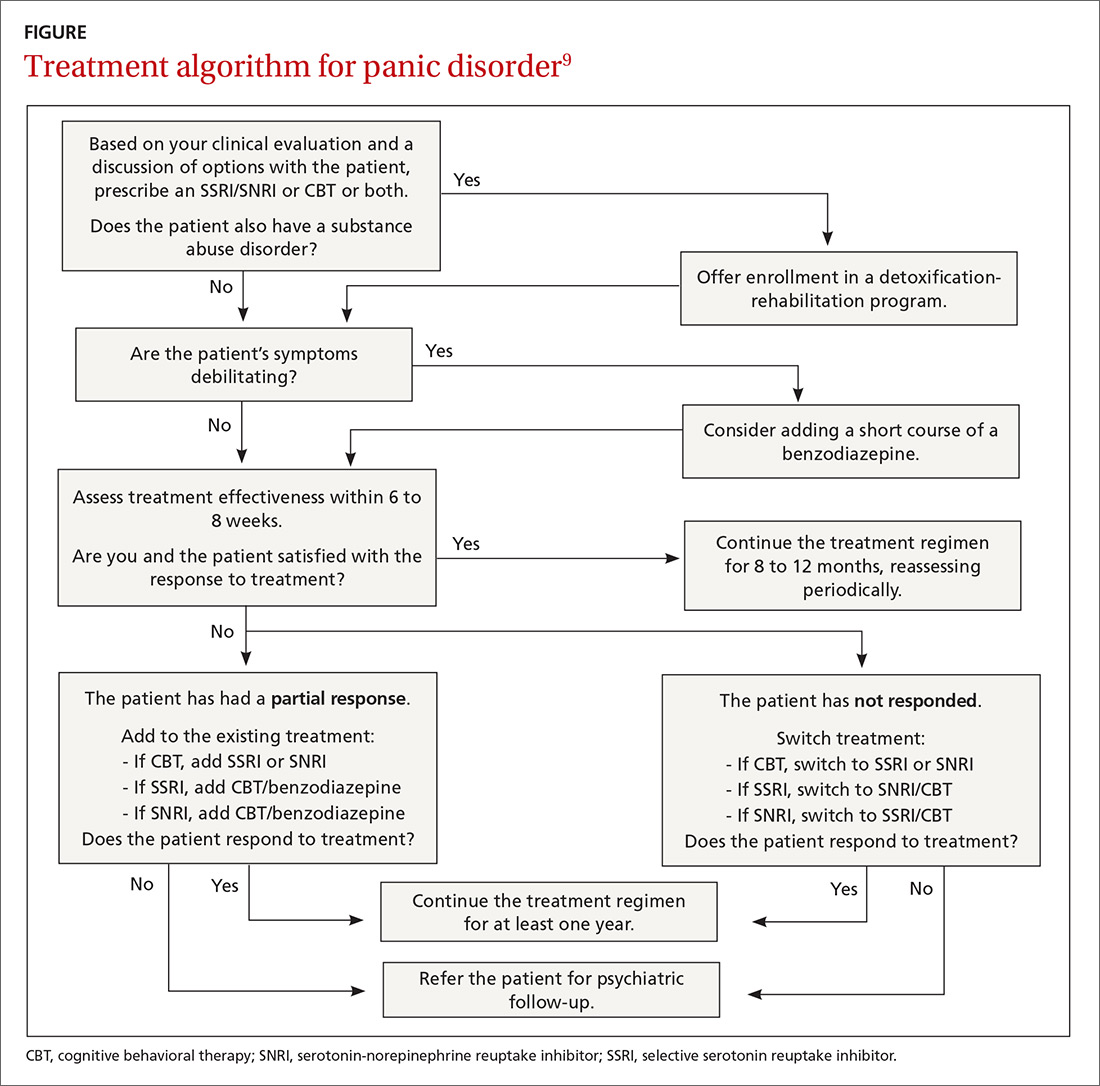
PD is a chronic disease with a variable course, but the long-term prognosis is good. PD is usually treated in an outpatient setting. Consider hospitalization if the patient is suicidal, if the potential for life-threatening withdrawal symptoms is high (as with alcohol or benzodiazepines), or if the symptoms are severely debilitating or attempted outpatient treatment is unsuccessful. Pharmacologic and psychotherapeutic interventions are used for PD (FIGURE9), although there is not enough evidence to recommend one vs the other or combination therapy vs monotherapy.9
CASE
For Ms. D, all medical test results came back negative, and the psychiatric assessment revealed that she met the DSM-5 criteria for panic disorder. Counting on the strength of their relationship, her physician talked to her about PD and discussed treatment options, which included counseling, medication, or both. Ms. D agreed to a referral for cognitive behavioral therapy (CBT) with a psychologist embedded at her physician’s primary care clinic and to begin taking medication. Her PCP started her on sertraline 25 mg/d.
In CBT, Ms. D’s psychologist taught her about “fight or flight” and explained that it was a normal physiologic response that could lead to panic. Ms. D. learned to approach her physical symptoms in a different way, and how to breathe in a way that slowed her panic reaction.
Consider SSRIs and SNRIs
First-line medication is a selective serotonin reuptake inhibitor (SSRI) or a serotonin-norepinephrine reuptake inhibitor (SNRI) due to the better tolerability and lower adverse effect profile of these classes compared with the tricyclic antidepressants or monoamine oxidase inhibitors. MAOIs are usually reserved for patients in whom multiple medication trials have failed.
Special considerations. American Psychiatric Association guidelines advise starting with a very low dose of an SSRI or SNRI, such as paroxetine 10 mg/d (although many clinicians start lower, at 5 mg/d), to avoid hypersensitivity reactions. Gradually titrate the dose upward within 3 to 7 days after initiation until a therapeutic dose is reached over 2 to 6 weeks. Schedule follow-up visits for every one to 2 weeks at the beginning of treatment and every 2 to 4 weeks until the therapeutic dose is reached. Assess safety/suicidality at each visit.
Keep in mind that the onset of therapeutic effect is between 2 and 4 weeks, but that clinical response can take up to 8 to 12 weeks. Continue pharmacotherapy for at least one year. When discontinuing the medication, taper it slowly, and monitor the patient for withdrawal symptoms and recurrence of PD.9
Consider adding a benzodiazepine if symptoms are debilitating.9 Keep in mind, though, that the potential for addiction with these medications is high and they are intended to be used for only 4 to 12 weeks.8 Onset of action is within the first week, and a scheduled dosing regimen is preferred to giving the medication as needed. The starting dose (eg, clonazepam 0.25 mg bid)9 may be increased 3 to 5 days following initiation.
The evidence supports the use of CBT for panic disorder
CBT is an evidenced-based treatment for panic disorder.10-13 Up to 75% of patients treated with CBT are panic free within 4 months.10 Other techniques proven effective are progressive muscle relaxation training, breathing retraining, psycho-education, exposure, and imagery.14
Treatment with medications and CBT either combined or used individually is effective in 80% to 90% of cases.15 CBT has been shown to decrease the likelihood of relapse in the year following treatment.15 Good premorbid functioning and a brief duration of symptoms increase the likelihood of a good prognosis.15
WHEN TO REFER TO A PSYCHIATRIST
Consider referral to a psychiatrist when patients have a comorbid psychiatric condition that complicates the clinical picture (eg, substance abuse disorder), if the diagnosis is uncertain, or if the patient does not respond to one or 2 adequate trials of medication and psychotherapy. Although psychiatric follow-up is sometimes difficult due to a lack of psychiatrist availability locally, it is a best-practice recommendation.