CASE A 40-year-old man came to our office slightly agitated. He had an acute illness that was minor in nature. However, he was not interested in answering my questions or undergoing a physical exam. The more I tried to proceed with the visit, the more agitated he became—pacing the room, muttering, avoiding eye contact. I was uncomfortable and knew that the situation could quickly escalate if it was not brought under control.
What steps would you take if this were your patient?
The scene described above occurred several years ago, but more recently, one of the institutions in my (TIM) area was affected by a shooter in the workplace. The apprehension felt by all of us who were on the periphery paled in comparison to what was experienced by those at the scene. The outcome was horrific. Communicating with those directly involved during, and immediately after, the event was heart-wrenching. The trauma that they continue to relive is unimaginable, and some are not yet able to return to work.
Situations involving agitated patients are not uncommon in health care settings, although ones that escalate to the level of a shooting are. And no matter where on the spectrum an incident involving an agitated patient falls, it can leave those involved with various levels of physical, emotional, and psychological harm. It can also leave everyone asking themselves: “How can I better prepare for such occurrences?”
This article offers some answers by providing tips and guidelines for handling agitated and/or violent patients in various settings.
Defining the problem, assessing its severity
Between 2011 and 2013, workplace assaults ranged from 23,540 and 25,630 annually, with 70% to 74% occurring in health care and social service settings.1,2
Agitation is defined as a state that may include inattention, disinhibition, emotional lability, impulsivity, motor restlessness, and aggression.3,4 Violence in a clinical setting may be seen as an extreme expression of agitation sufficient enough to cause harm to an individual or damage to an object.5,6
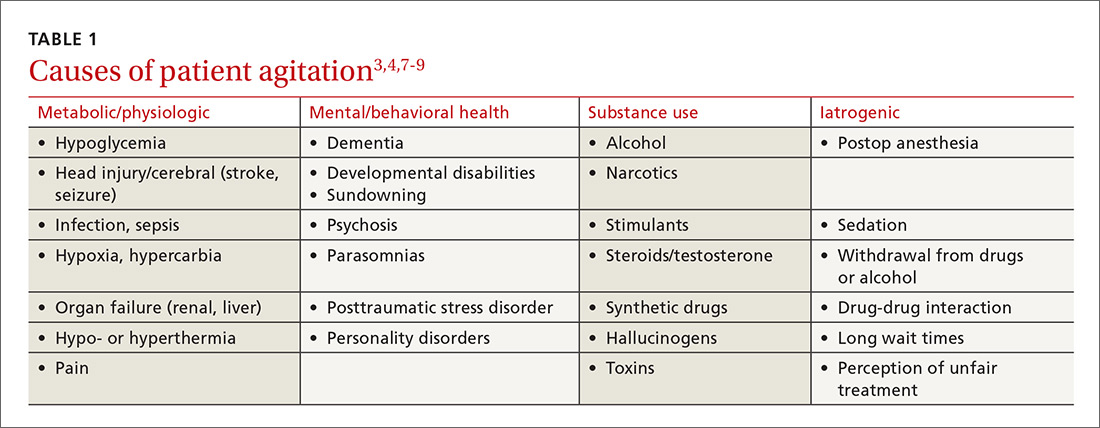
The causes of agitation can be grouped into categories: those due to a general medical condition, those due to a psychiatric condition, and those due to drug intoxication and/or withdrawal.7 We have chosen to add a fourth category—iatrogenic (see TABLE 13,4,7-9). They are not distinct categories, as there is sometimes overlap among areas.
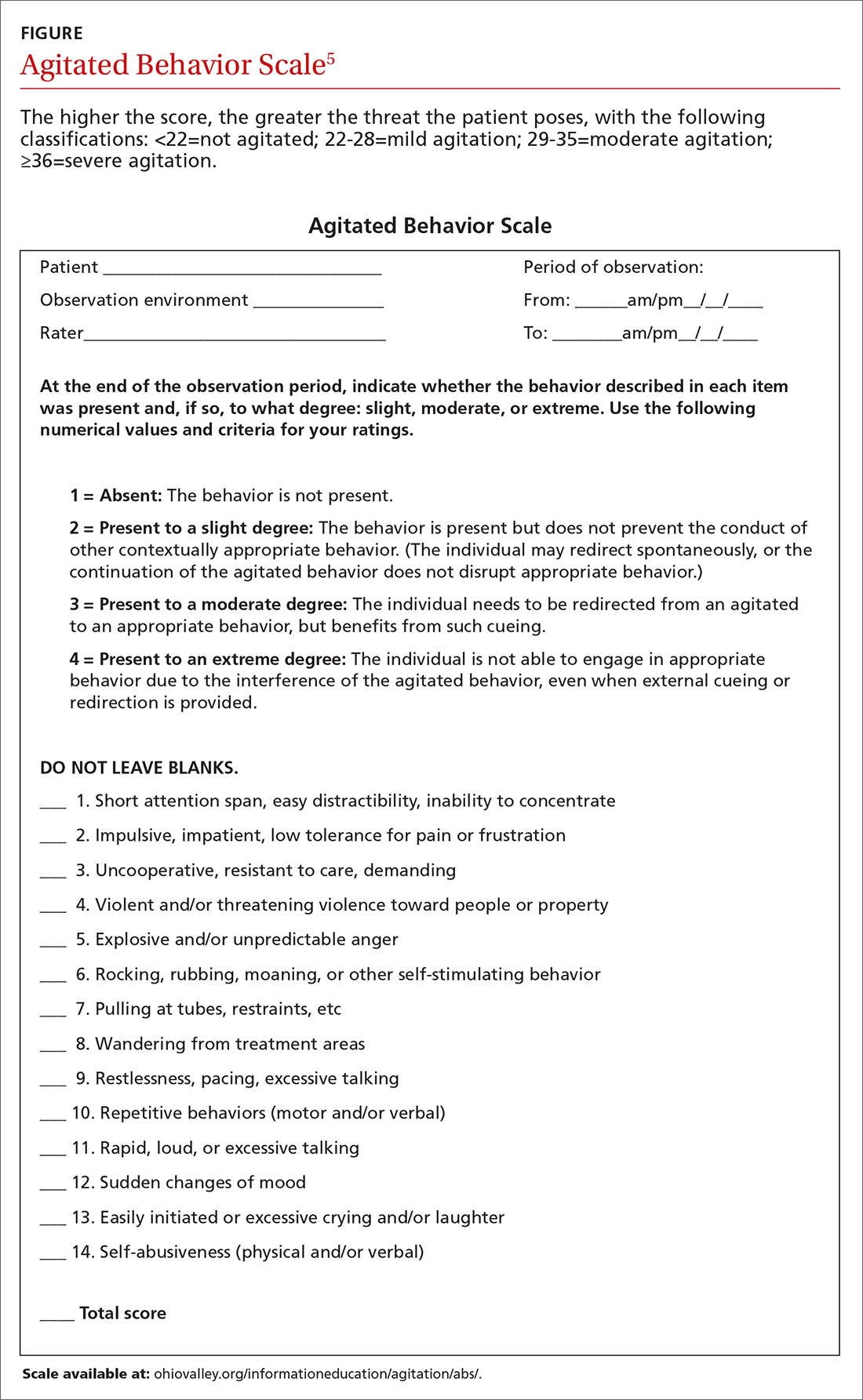
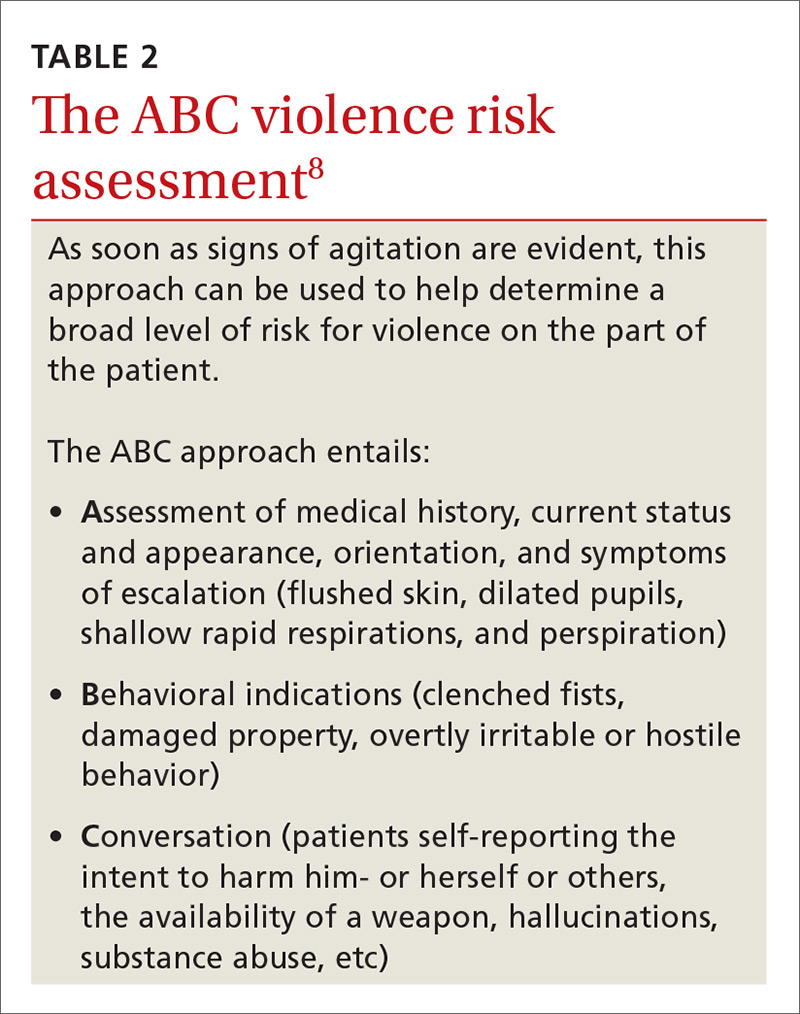
Determining the level of agitation. Various scales and approaches can help determine the level of agitation in a patient (eg, the Agitated Behavior Scale [ABS; FIGURE];5 the Behavioral Activity Rating Scale [BARS]10) and the risk for violence (eg, the ABC violence risk assessment, TABLE 28).
Scales like the ABS should be employed as soon as a patient shows signs of agitation sufficient to warrant intervention. The idea is for the family physician (FP) to be familiar enough with the tool to be able to mentally check it off, fill it out when time permits, and keep it in the patient’s chart. The first version of the form serves as a baseline so that if care is handed off to another provider, that provider can monitor whether signs and symptoms are improving or worsening.
Setting often drives the solution
Much of the evidence-based research on managing patient agitation and violence stems from inpatient psychiatric and emergency department (ED) settings. To make other health care providers aware of the experience gained in those settings, the American Association for Emergency Psychiatry created Project BETA (Best Practices in Evaluation and Treatment of Agitation). This project is designed to help promote consistency across health care settings and specialties in the way clinicians respond to agitated patients and to emphasize for all health care providers the availability of more than just pharmacologic approaches.7