CASE
Patrick S, an 85-year-old man with multiple medical problems, was brought to his primary care provider after being found at home with altered mental status. His caretaker reported that Mr. S had been using extra blankets in bed and sleeping more, but he hadn’t had significant outdoor exposure. Measurement of his vital signs revealed tachycardia, tachypnea, hypotension, and a rectal temperature of 32°C (89.6°F).
How would you proceed with the care of this patient?
What is accidental hypothermia?
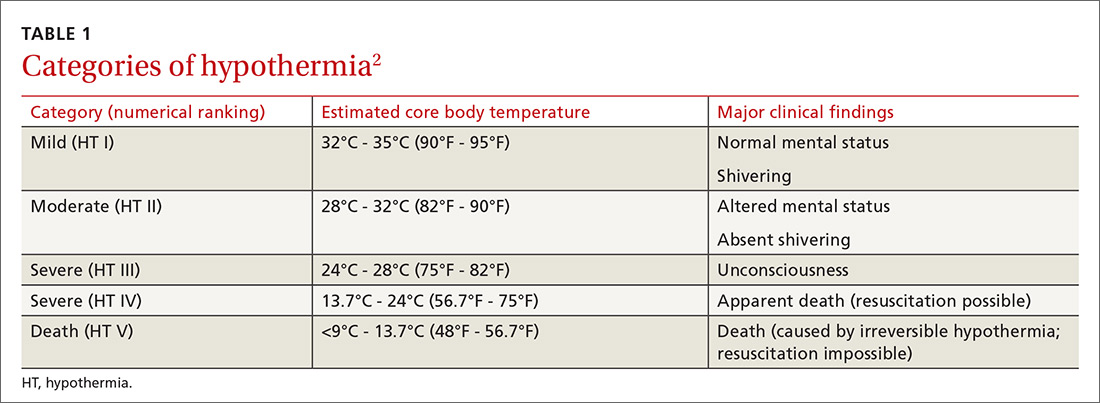
Accidental hypothermia is an unintentional drop in core body temperature to <35°C (<95°F). Mild hypothermia is defined as a core body temperature of 32°C to 35°C (90°F - 95°F); moderate hypothermia, 28°C to 32°C (82°F - 90°F); and severe hypothermia, <28°C (<82°F).1
The International Commission for Mountain Emergency Medicine divides hypothermia into 5 categories, emphasizing the clinical features of each stage as a guide to treatment (TABLE 1).2 These categories were adopted to help prehospital rescuers estimate the severity of hypothermia using physical symptoms. For example, most patients stop shivering at approximately 30°C (86°F)—the “moderate (HT II)” category of hypothermia—although this response varies widely from patient to patient. Notably, there are reports in the literature of survival in hypothermia with a temperature as low as 13.7°C (56.7°F) and with cardiac arrest for as long as 8 hours and 40 minutes, although these events are rare.3
Each year, approximately 700 deaths in the United States are the result of hypothermia.4 Between 1995 to 2004 in the United States, it is estimated that 15,574 visits were made to a health care provider or facility for hypothermia and other cold-related concerns.5 Based on reports in the international literature, the incidence of nonlethal hypothermia is much greater than the incidence of lethal hypothermia.5 Almost half of deaths from hypothermia are in people older than age 65 years; the male to female ratio is 2.5:1.1
Variables that predispose the body to temperature dysregulation include extremes of age, comorbid conditions, intoxication, chronic cold exposure, immersion accident, mental illness, impaired shivering, and lack of acclimatization.1 The most common causes of death associated with hypothermia are falls, drownings, and cardiovascular disease.4 In a 2008 study, hypothermia and other cold-related morbidity emergency department (ED) visits required more transfers of patients to a critical care unit than any other reason for visiting an ED (risk ratio, 6.73; 95% confidence interval, 1.8-25).5 Mortality among inpatients whose hypothermia is classified as moderate or severe reaches as high as 40%.3
More than just cold-weather exposure
Accidental hypothermia occurs when heat loss is superseded by the body’s ability to generate heat. It commonly happens in cold environments but can also occur at higher temperatures if the body’s thermoregulatory system malfunctions.
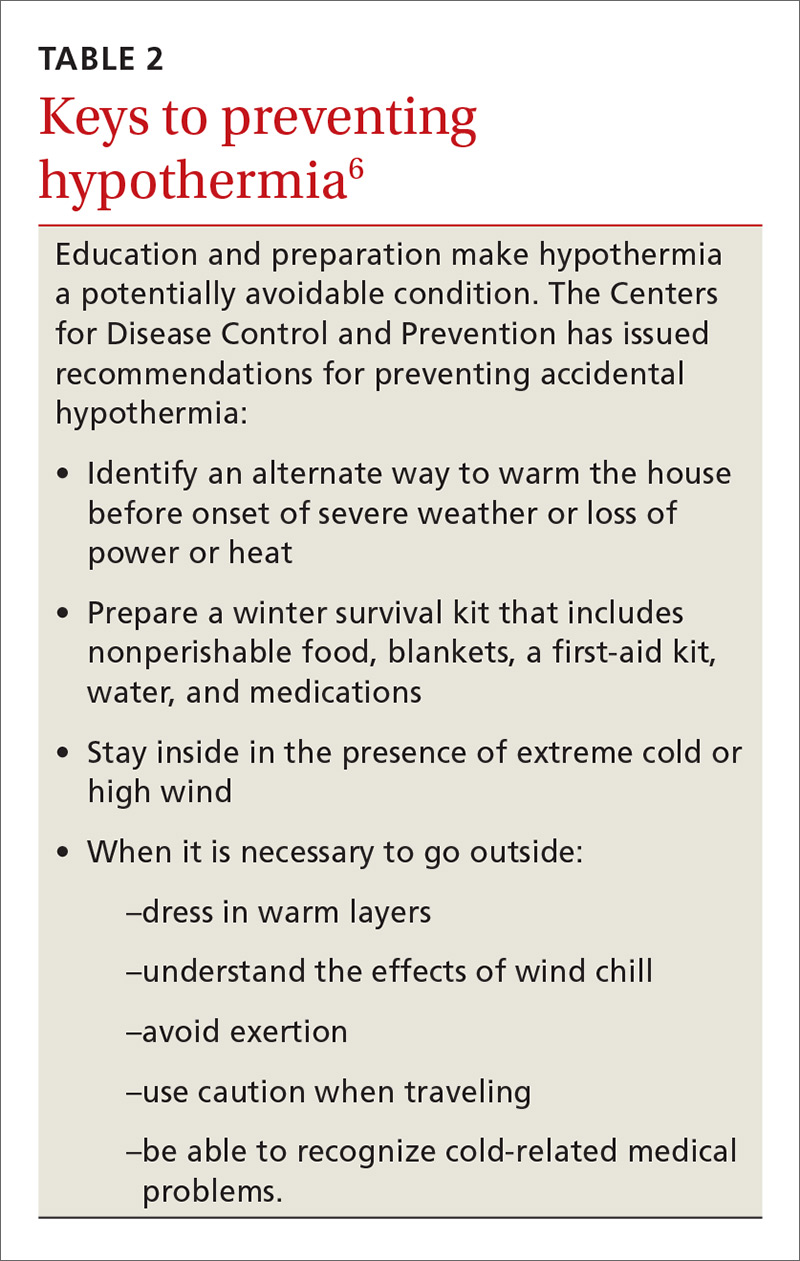
Environmental or iatrogenic factors (ie, primary hypothermia), such as wind, water immersion, wetness, aggressive fluid resuscitation, and heat stroke treatment can make people more susceptible to hypothermia. Medical conditions (ie, secondary hypothermia), such as burns, exfoliative dermatitis, severe psoriasis, hypoadrenalism, hypopituitarism, hypothyroidism, acute spinal cord transection, head trauma, stroke, tumor, pneumonia, Wernicke’s disease (encephalopathy), and sepsis can also predispose to hypothermia.1 Drugs, such as ethanol, phenothiazines, and sedative–hypnotics may decrease the hypothermia threshold.1 (For information on preventing hypothermia, see TABLE 2.6)