Electrocardiography. An electrocardiogram is essential to evaluate for arrhythmias. Findings associated with hypothermia are prolongation of PR, QRS, and QT intervals; ST-segment elevation, T-wave inversion; and Osborn waves (J waves), which represent a positive deflection at the termination of the QRS complex with associated J-point elevation.8 Osborn waves generally present when the core body temperature is <32°C (89.6°F) and become larger as the core body temperature drops further.3
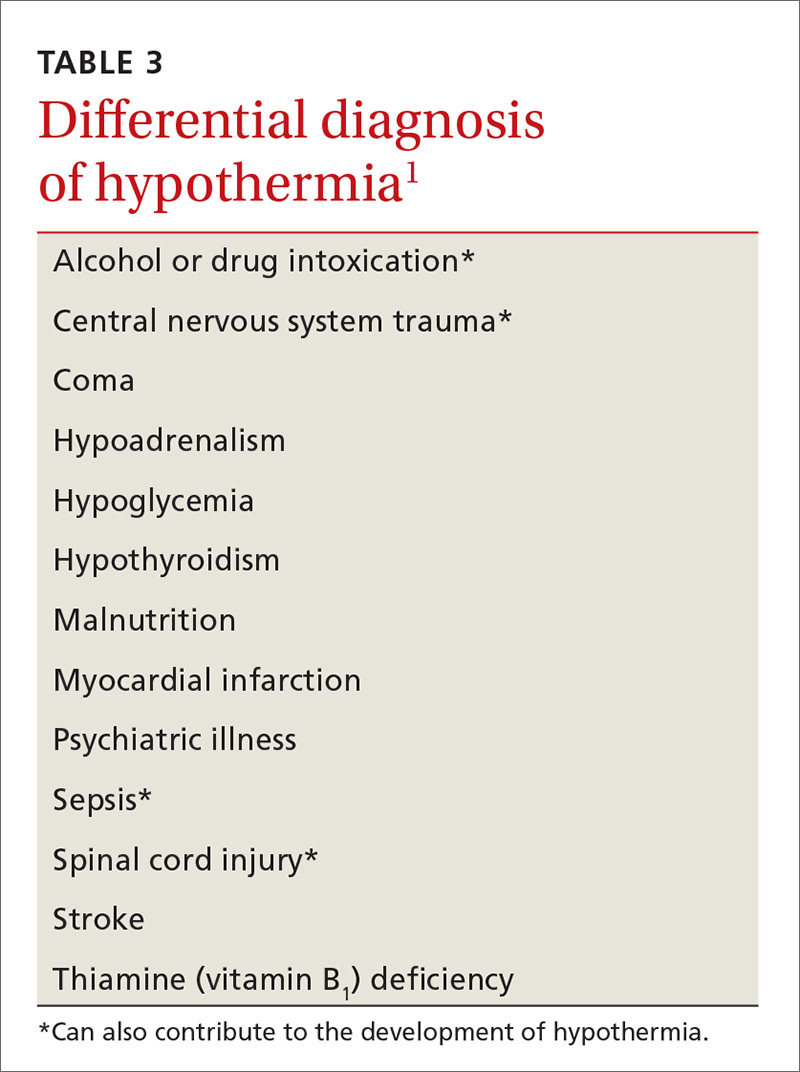
Differential diagnosis. Hypothermia is most commonly caused by environmental exposure, but the differential diagnosis is broad: many medical conditions, as well as drug and alcohol intoxication, can contribute to hypothermia (TABLE 31).
Treatment: Usually unnecessary, sometimes crucial
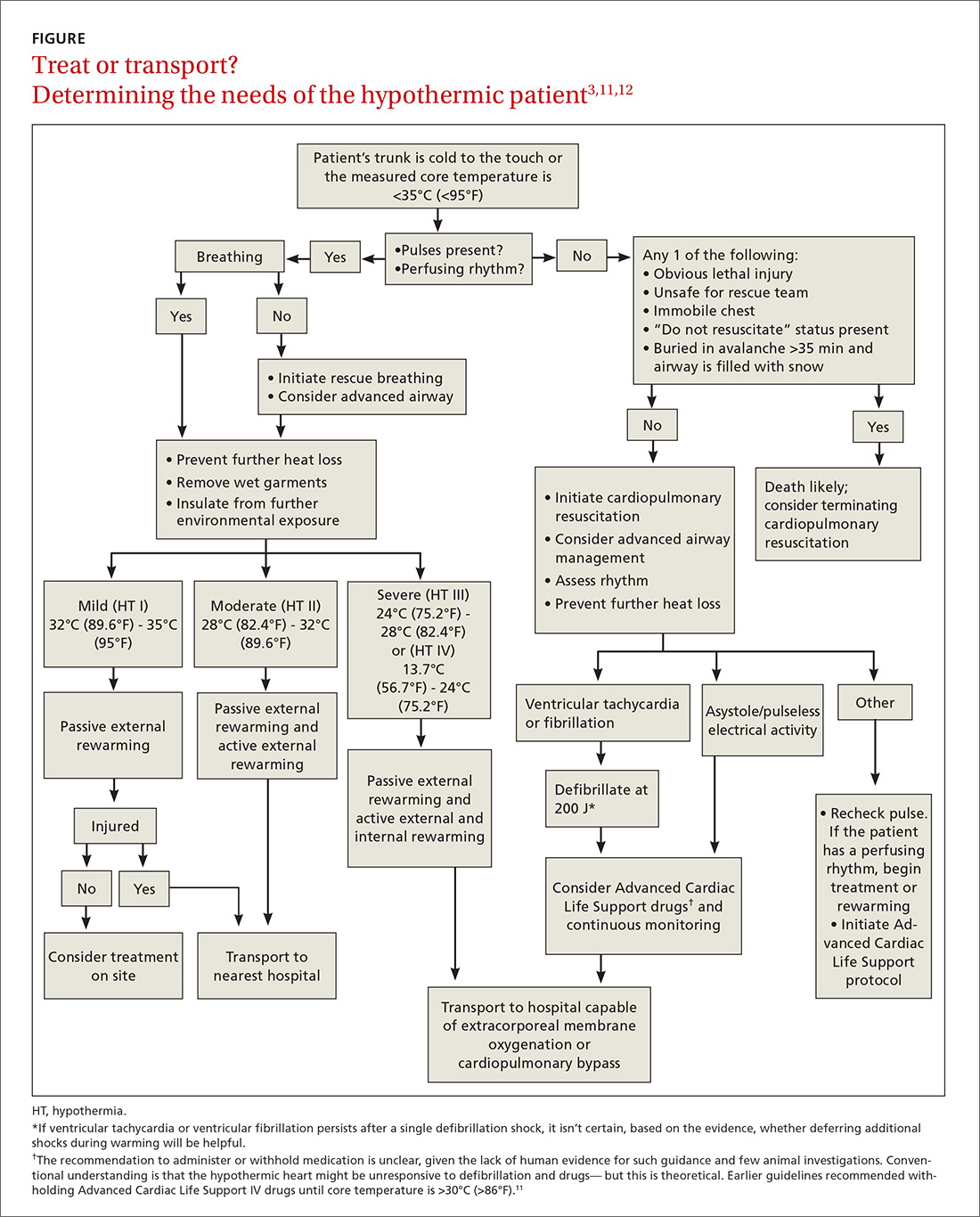
Most patients with mild hypothermia recover completely with little intervention. These patients should be evaluated for cognitive irregularities and observed in the ED before discharge.9 Moderate and severe hypothermia patients should be assessed using pre-hospital protocols and given cardiopulmonary resuscitation (CPR) for cardiac arrest. Pre-hospital providers should rely more on symptoms in guiding their treatment response because core body temperature measurements can be difficult to obtain, and the response to a drop in core body temperature varies from patient to patient.10
Early considerations: Airway, breathing, circulation (ABC)
A first responder might have difficulty palpating the pulse of a hypothermic patient if that patient’s cardiopulmonary effort is diminished.9 This inability to palpate a pulse should not delay treatment unless the patient presents with lethal injury; the scene is unsafe; the chest is too stiff for CPR; do-not-resuscitate status is present; or the patient was buried in an avalanche for ≥35 minutes and the airway is filled with snow (FIGURE3,11,12). Pulse should be checked carefully for 60 seconds. If pulses are not present, CPR should be initiated.
Prevention of further heat loss should begin promptly for hypothermic patients who retain a perfusing rhythm.11 Lifesaving interventions, such as airway management, vascular access for volume replenishment, and defibrillation for ventricular tachycardia or ventricular fibrillation should be carried out according to Advanced Cardiac Life Support protocols.11 Patients in respiratory distress or incapable of protecting their airway because of altered mental status should undergo endotracheal intubation. Fluid resuscitation with isotonic crystalloid fluids, warmed to 40°C (104°F) to 42°C (~107°F) and delivered through 2 large-bore, peripheral intravenous (IV) needles, can be considered.
Special care should be taken when moving a hypothermic patient. Excessive movement can lead to stimulation of the irritable hypothermic heart and cause an arrhythmia.