LONDON – Patients with rheumatoid arthritis who have had total joint replacement are not at greater risk of joint infection if they use biologic agents when compared with conventional disease-modifying drugs.
New data from the German biologics register RABBIT (Rheumatoid Arthritis Observation of Biologic Therapy) show that the overall rate of periprosthetic joint infection is low, at 1%, and remains low regardless of the treatment type.
"A lot of patients with RA have to undergo joint replacement," said Dr. Anja Strangfeld of the German Rheumatism Research Center Berlin, where the biologics register is based.
During an interview, Dr. Strangfeld noted that concern has been voiced about the use of anti-tumor necrosis factor (TNF) agents in patients who need a joint replacement because of the possibility of an increased risk of serious infections.
"It was also thought that in people who already have prostheses, a joint infection will be more likely to occur after starting biologic treatment, especially with anti-TNF agents," Dr. Strangfeld observed.
"The hypothesis was that microorganisms could enter the joint during the surgery [and] form a protective biofilm," but this biofilm might get disrupted when anti-TNF treatment is started, she said. This disruption allows the infective agent to spread and cause infection.
However, of 1,495 total joint replacements in 1,013 patients, very few got infected.
"In our whole register, we only found 15 periprosthetic joint infections, and this means that 1% of the procedures got infected. That’s good news, as it seems that there is not an increased risk for patients," Dr. Strangfeld said.
Until May 2010, 7,536 patients with RA were included in the RABBIT database and were treated with conventional disease-modifying antirheumatic drugs (DMARDs), anti-TNFs, or other biologic agents (tocilizumab, rituximab, abatacept).
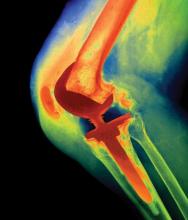
Only total replacements of the hip, knee, shoulder, or ankle were included in the analysis, and patients had received joint prostheses both before and after enrollment. The mean exposure to biologic therapy before joint surgery was 2.7 years.
There was no significant difference between the percentage of joints that became infected in patients treated with DMARDs versus those treated with anti-TNF agents (1.5% vs. 1.5%; P = .077)
There was also no significant difference observed among individual anti-TNF drugs, with rates of 1.5%, 1.4%, and 0.9% for adalimumab, etanercept, and infliximab, respectively.
These incidence rates are in line with data from Danish and Finnish arthroplasty registries, in which infection rates of 0.7% and 1.3% have been reported.
In patients treated with tocilizumab, rituximab, or abatacept, no periprosthetic infections occurred, although the number of patient-years of observation were much lower than that for anti-TNFs and DMARDS.
The microorganism responsible for the joint infection was reported in only 10 cases – with Staphylococcus spp. being the most common culprit (6 cases).
When asked whether patients who underwent joint replacement surgery might have to take antibiotic prophylaxis, Dr. Strangfeld noted that this was something that the current analysis could not determine but would be interesting to look at.
These findings suggest that patients who need to have a joint replacement and who are already being treated with a biologic agent should have no great cause to worry about contracting an infection.
"For patients who already have a joint replacement, they also don’t have to worry that much if they start a biologic agent," Dr. Strangfeld said.
RABBIT is supported by a joint, unconditional grant from the following German manufacturers of biologic agents: Abbott, Amgen/Swedish Orphan Biovitrum, Bristol-Myers Squibb, Essex/MSD, Pfizer, Roche, and UCB. Dr. Strangfeld had no personal financial disclosures.