TABLE 1
Demographic and baseline characteristics of the study participants
| Intrathecal narcotics (n = 63) | Epidural (n = 19) | P | |
|---|---|---|---|
| Demographic characteristics | |||
| Age (years) | 28.4 ± 5.7 | 30.7 ± 3.6 | .10 |
| Nulliparous (%) | 63.5 | 47.4 | .21 |
| Caucasian (%) | 74.6 | 84.2 | .39 |
| Marital status single (%) | 20.6 | 10.5 | .32 |
| Employer-paid insurance (%) | 81.0 | 94.7 | .15 |
| Gestational age (weeks) | 39.5 ± 1.1 | 39.4 ± 1.4 | .69 |
| Baseline characteristics | |||
| Previous ITNs or epidural (%)* | 65.2 | 80.0 | .40 |
| Cervical dilation (cm) | |||
| On admission | |||
| Parity 0 | 2.6 ± 1.3 | 2.8 ± 1.3 | .75 |
| Parity > 0 | 2.6 ± 1.3 | 1.7 ± 0.9 | .07 |
| At analgesic placement | |||
| Parity 0 | 4.4 ± 1.4 | 4.1 ± 0.9 | .46 |
| Parity > 0 | 4.6 ± 1.4 | 3.8 ± 1.1 | .09 |
| Negative station at analgesic placement (%) | 51.7 | 63.2 | .38 |
| ROM prior to placement (%) | 55.6 | 68.4 | .32 |
| Oxytocin use prior to placement (%) | 30.2 | 36.8 | .59 |
| VAS at time of placement | 65.3 ± 29.0 | 67.8 ± 18.5 | .73 |
| Data are presented as mean ± SD or as percent. | |||
| *Previous ITNs or epidural analgesia includes parous women only. | |||
| ITNs, intrathecal narcotics; ROM, rupture of membranes; VAS, visual analog scale. | |||
Analgesia
Two women who initially received ITNs were subsequently given an epidural, but they remained in the ITN group for analysis. Eight women (13%) in the ITN group required a second intrathecal injection, and only 5 (8%) received a pudendal nerve block in the second stage of labor.
Pain
Women receiving epidural analgesia had significantly lower mean pain scores for the first and the second stages of labor, as well as for the overall postpartum assessment Table 2. Adjusting with multivariate regression did not significantly alter the results. For women in both groups, the mean postpartum overall VAS scores exceeded both the first-and second-stage scores measured during labor and appeared to reflect the higher of the 2.
From the standpoint of “analgesic success,” the odds of having a VAS score ≤ 30 throughout the first stage of labor were 24 times greater for women receiving epidural analgesia than for those receiving ITNs (Table 2, adjusted odds ratio [OR] = 24.4, 95% CI = 5.1–116.3, number needed to treat [NNT] = 2). Of note, however, VAS scores remained in the “zone of analgesic success” for 12 women (20% of the ITN group) who delivered within 3 hours of receiving ITNs. In the second stage, the odds of having successful analgesia were 7 times higher for women receiving epidural analgesia (adjusted OR = 7.1, 95% CI = 1.7–29.1, NNT = 3).
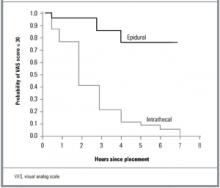
The difference in the duration of effective pain relief was also highly significant (Figure 1, log-rank test, P < .001). For women receiving ITNs, the median duration of effective pain relief in the first stage of labor was between 60 and 120 minutes. Continuous epidural infusion, by contrast, maintained successful analgesia for most women for the entire duration of the first stage.
TABLE 2
Pain ratings and overall satisfaction with pain management
| Outcome | Intrathecal narcotics (n = 63) | Epidural (n = 19) | Adjusted differences |
|---|---|---|---|
| Stage 1 VAS | 35.1 ± 20.6 | 9.7 ± 9.6 | 24.7* |
| Stage 2 VAS | 58.5 ± 33.7 | 23.1 ± 23.5 | 42.0* |
| Overall VAS | 61.8 ± 24.9 | 24.6 ± 30.0 | 37.6* |
| Overall satisfaction with pain management (5 = very satisfied) | 3.9 ± 0.9 | 4.7 ± 0.5 | –0.8† |
| Data are presented as mean ± SD. Differences are adjusted for maternal age, parity, previous spinal analgesic use, cervical dilation at time of placement, oxytocin use prior to placement, and weight of baby. | |||
| Differences are *P < .001 or † P = .001. | |||
| VAS, visual analog scale. | |||
FIGURE 1
Kaplan-Meier analysis of the time to analgesic failure (VAS score > 30)
Satisfaction
Although women in both groups expressed overall satisfaction with the way their pain was controlled during labor, there were significant differences between groups. On a Likert scale where 5 = very satisfied, 4 = satisfied, and 3 = neutral, the mean rating for women in the epidural group was 4.7, compared to 3.9 for women receiving ITNs (P = .001). High levels of satisfaction correlated significantly with lower postpartum overall VAS scores (r = 20.50, P < .001). There were similar relationships between overall satisfaction and mean VAS scores in the first stage (r = 2.35, P = .002) and the second stage (r = 20.25, P = .040) of labor.
Side effects
Women receiving ITNs were significantly more likely to experience itching than were those receiving epidural analgesia (P < .001; Figure 2). In fact, 95% of the ITN group experienced itching, although nearly two thirds indicated that the symptom was mild or brief and did not interfere with the overall birthing experience. Nausea and vomiting were reported slightly more often in the ITN group, but the difference was not statistically significant. Women receiving epidural analgesia were significantly more likely to experience headaches (P < .001) and an inability to walk (P < .001). They also reported more difficulty with urination (P = .15) and with pushing (P = .23), neither of which reached statistical significance. None of the women reporting headaches were diagnosed as having postdural puncture headaches, and none required a blood patch for treatment. On the side effect severity index, 29% of women in the ITN group reported at least 1 “very bad” symptom, compared to 17% in the epidural group (P = .30).