Q: What causes of sudden unilateral vision loss would you consider? What would you do next?
Your examination yields the following:
Medical history
- Borderline hypertension
- Hyperlipidemia (was on a medication but discontinued it on his own)
- Smoking 25 pack-years; quit 2 years ago
- Occasional alcohol intake
- No medications
- Electrical contractor by trade
- Parents living and well; siblings have hypertension but no other illnesses.
Review of systems
Negative except for occasional nasal congestion and low back pain.
Physical examination
- Alert male in no distress. Blood pressure, 146/86 mm Hg; weight, 85 kg; heart rate, 80; respiratory rate, 20; temperature normal; skin warm and dry.
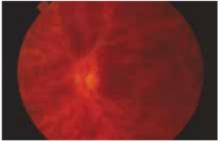
- Head, eyes, ears, nose, throat: pupils are equal, round, and reactive to light and accommodation; extraocular movement intact; retinal exam is depicted in the Figure. Tympanic membranes, throat, and neck normal; carotids normal.
- Heart and lung exam unremarkable. Spleen questionably palpable. Extremities normal. Neurologic exam normal, except for eye findings.
FIGURE
Retinal exam
Referring to Harrison’s Textbook of Medicine, you find the following entry:
“Venous occlusion of the retina is often idiopathic, but hypertension, diabetes, and glaucoma are prominent risk factors. The benefit of treatment with anticoagulants is unproven and carries the risk of hemorrhage into the vitreous. Polycythemia, thrombocythemia, or other factors leading to an underlying hypercoagulable state should be corrected.”1
You also reviewed information from UpToDate, which revealed a British article linking retinal venous occlusion with an increased risk of cardiovascular disease. It recommends that clinicians use an algorithm to determine the appropriate treatment.2 Additional research noted various interventions for the venous occlusion itself, but none had sufficient numbers to be considered reliable in recommending treatment.
You have identified 3 problems, 2 of which you deal with regularly and a third that requires consultation:
- Hypertension
- Hyperlipidemia
- Central retinal venous occlusion (CRVO) (rule out underlying hypercoagulable state).
Ophthalmologist’s report
An ophthalmologist confirms a diagnosis of left retinal vein occlusion, and recommends a period of observation, to see if vision returns. The opthalmologist also asks the patient to return to you for an investigation of possible underlying medical conditions.
Further primary care evaluation
The patient’s history suggests nothing that would inhibit a return of vision. Findings on the physical examination are unchanged except for the left fundus. The patient is quite concerned about another “stroke,” particularly in the other eye. He wants a guarantee he will be okay.
Laboratory evaluation:
- Complete blood count, normal
- Urea nitrogen (BUN), 20 mg/dL
- Creatinine kinase, 1.2 mckat/L
- Liver functions within normal limits
- Glucose, 86 mg/dL
- Cholesterol, 230 mg/dL
- Triglycerides, 186 mg/dL
- HDL, 41 mg/dL; LDL, 136 mg/dL
- Total serum protein levels, normal.
Additional time was required by the family physician to coordinate care of this patient. A team management code (99361 for 30 minutes and 99362 for 60 minutes) may not be billed on the same day as an e/m code, as carriers bundle this into the e/m. In addition, most carriers do not pay for the 99361 or 99362 codes. Therefore, the conference should ideally occur the day of an e/m code and be documented with that service. In this instance, the care occurred over several days, so no additional billing was allowed for team management.
Details of central retinal venous occlusion
You assure the patient you will coordinate care with the ophthalmologist, who subsequently offers the following summary about CRVO:
- For most patients with CRVO, vision decreases to 20/100, 20/200, or worse, usually permanently if the occlusion is indeed venous and not arterial as well. If the condition is secondary to ischemia, vision is usually limited to 20/300 or worse, permanently.
- Most patients want their vision “fixed” right away, but that is usually not possible. Hypertension control is most important. Uncommon causes include polycythemia vera, emphysema, sickle cell disease, multiple myeloma, macroglobulinemia, hyperproteinemia, cystic fibrosis of the pancreas, and peritoneal dialysis. Occasionally, it can occur secondary to hypotension, as from a ruptured aortic aneurysm, delivery-associated blood loss, or surgical trauma.
- Hypertension and other atherosclerotic risk factors must be controlled. Treatment with platelet inhibitors is often recommended and glaucoma control is very important, especially for African American patients. Chronic open-angle glaucoma can present as CRVO, and results can be devastating. African Americans are about 100 times more likely than Caucasians to have glaucoma (1/7 vs 3/2000).