- In low-risk patients, the physician should conduct a thorough history and physical examination. Routine laboratory testing may be useful, but further evaluation for underlying malignancy is unnecessary (B).
- Test for disorders associated with hypercoagulability under the following circumstances: when a thrombotic event occurs in a person younger than age 50; if a patient has a family history of venous thromboembolism; or if there are recurrent episodes of unexplained venous thromboembolism (C).
- When homocysteine levels are elevated in the presence of factor V Leiden or the prothrombin gene G20210A mutation, risk of recurrent thrombosis appears to be increased beyond the r isk associated with any one defect alone (B).
In which direction, and how aggressively, should the investigation proceed when common and obvious causes of venous thromboembolism—recent surgery, trauma, immobilization, or malignancy—are absent from a patient’s history?
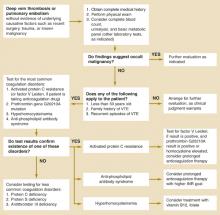
Two causes of hypercoagulability warrant consideration: occult malignancy and coagulation disorders resulting in thrombophilia. This review provides guidance on diagnostic testing and extent of the work-up, summarized in an algorithm (Figure).
FIGURE
Evaluating idiopathic venous thromboembolism
Malignancy and Venous Thromboembolism
Armand Trousseau first described the association between VTE and cancer nearly 150 years ago.5 For patients with known malignancy, a search for other possible causes of thrombosis is seldom needed (strength of recommendation [SOR]=B).
However, for individuals with idiopathic DVT or pulmonary embolism (PE), the clinician’s dilemma is in deciding how aggressively to look for occult malignancy. In a prospective study of 738 patients with objectively verified symptomatic deep vein thrombosis (DVT), cancer was the most common underlying cause and emerged as a major predictor of recurrent thrombotic events.6 Unfortunately, no laboratory test predicts occult cancer among patients with VTE.7
Risk of malignancy in per spective
Evidence of malignancy is usually discovered when taking a patient’s history and conducting a physical examination. Searching beyond the history and physical exam is seldom revealing.
In 1992, Prandoni and colleagues8 published a report of a study of 262 patients with symptomatic DVT, 250 of whom were followed for 2 years. One hundred seven patients had recognized nonmalignant risk factors for DVT and were not evaluated for cancer. Of the 155 patients with idiopathic venous thrombosis, 5 (3.3%) were discovered to have occult carcinoma. Malignancy was suggested in 4 of the 5 by history or physical examination.
In a similar study, Hettiarachchi et al9 evaluated 400 patients with confirmed DVT and found 70 (18%) had a diagnosis of cancer at the time of presentation. Of the remaining 326 patients (4 were lost to follow-up), 189 had recognized risk factors for DVT, 3 (1.6%) of whom were also found to have cancer; and 137 patients had unexplained DVT, 10 of whom (7.3%) were found to have occult carcinoma. As in the Prandoni study, most of the patients subsequently discovered to have cancer (10 of 13, 77%) had suggestive clinical findings in the history or physical examination.9
Venous thromboembolism and specific types of cancer
Two large, retrospective epidemiologic studies reviewed cases of thousands of patients in the Danish and Swedish National Patient Registries.10,11 Investigators for these studies found an approximately 30% increase in the diagnosis of cancer among patients with VTE compared with the general population. Because of their large size, both of these studies were able to demonstrate a significant association between thrombosis and pancreatic, liver, and ovarian cancers.
For liver and pancreatic cancers, consensus opinion suggests that early diagnosis does not change prognosis. Similarly, although some experts recommend ultrasound and Ca-125 testing to investigate possible ovarian cancer, no data support use of these tests in ovarian cancer screening.12
An evaluation of the Danish National Registry data has suggested that cancer diagnosed at the time of, or within a year of, the diagnosis of VTE is usually advanced and is associated with a poor prognosis.13 Indeed, the authors of the Danish study concluded that for patients with VTE, “[our] pragmatic recommendation [is] to use only simple methods of screening and to look for cancer in patients with signs and symptoms of cancer.”13
Recommended work-up
We conclude the literature8-13 does not support an aggressive search for hidden cancer in a patient with idiopathic VTE (SOR=B). Routine evaluation should include a careful history and physical examination. Because of their low cost, reliability, and ready availability, studies such as a complete blood count, basic chemistry panel, liver function tests, and urinalysis may be considered (SOR=B ). Examples of findings during the initial history, physical exam, and laboratory studies that should prompt further evaluation include anorexia, weight loss, cough, abdominal bloating, unexplained anemia, hyponatremia, hematuria, and abnormal liver enzymes.