Diagnosis relies on pneumatic otoscopy
On physical exam, the patient will likely appear well. Otoscopic examination reveals fluid behind a normal or retracted tympanic membrane; the fluid is often clear or yellowish in color.
A subcommittee comprised of members of the American Academy of Pediatrics, American Academy of Family Physicians, and the American Academy of Otolaryngology-Head and Neck Surgery (AAP/AAFP/AAOHNS) published a clinical practice guideline in 2004 that delineates the current diagnosis and management of children between 2 months and 12 years of age with OME.17
Pneumatic otoscopy, which can reveal decreased or absent movement of the tympanic membrane (the result of fluid behind the membrane), is the primary diagnostic method recommended by the guideline. Tympanometry and acoustic reflectometry may also be used to make the diagnosis, especially when the presence of MEE is difficult to determine using pneumatic otoscopy.
CASE › Upon further discussion with the patient’s mother, you learn that the boy goes to day care 3 days a week and stays with his grandmother 2 days a week. His grandmother smokes outside of the home when he is staying with her.
After reviewing these risk factors with the mother (including the importance of smoking cessation for the grandmother), the mother asks if he needs antibiotics or a referral to a specialist for treating his OME.
How best to approach treatment
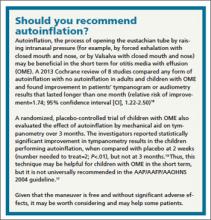
There are several management options to choose from, including watchful waiting, medication, and/or surgery. (Another option, autoinflation, which has shown some short-term benefits, is described in “Should you recommend autoinflation?”17-19.)
The goals of management are to resolve the effusion, restore normal hearing (if diminished secondary to the effusion), and prevent future episodes or sequelae. The most significant complication of OME is permanent conductive hearing loss, but tinnitus, cholesteatoma, or tympanosclerosis may also occur.
In most patients, OME resolves without medical intervention. If additional action is required, however, the following options may be explored.
Medication. While the AAP/AAFP/AAOHNS guideline recommends against routine antibiotics for OME,17 it does note that a short course may provide short-term benefit to some patients (eg, those for whom a specialist referral or surgery is being considered).
A separate meta-analysis found that antibiotics improve clearance of the effusion within the first month after treatment (rate difference [RD]=0.16; 95% confidence interval [CI], 0.03-0.29 in 12 studies analyzed), but effusion relapses were common, and no significant benefit was noted past the first month (RD=0.06; 95% CI, -0.03 to 0.14 in 8 studies).20
If you do use antibiotics, a 10- to 14-day course is preferred.17 Amoxicillin, amoxicillin-clavulanate and ceftibuten have been evaluated in separate clinical trials, but none has been clearly shown to have significant advantage over any other.21,22
Antihistamines, decongestants, and oral and intranasal corticosteroids have little effect on OME in children and are not recommended.17 A Cochrane review including 16 studies found that children receiving antihistamines and decongestants are unlikely to see their symptoms improve significantly, and many patients experience adverse effects from the medications23 (number needed to harm=9).
A randomized, double-blind trial involving 144 children <9 years of age with OME for at least 2 months evaluated 4 regimens involving amoxicillin alone or in combination with prednisolone. Children in the amoxicillin+prednisolone arms were significantly more likely to clear their effusions at 2 weeks (number needed to treat=6; P=.03), but not at 4 weeks (P=.12). At 4-month follow-up, effusions had recurred in 68.4% and 69.2% of those receiving amoxicillin+prednisolone and those receiving amoxicillin alone, respectively (P= .94).24
Surgery—or not? The AAP/AAFP/AAOHNS guideline recommends physicians perform hearing testing when OME is present for 3 months or longer, or at any time if language delay, learning problems, or a significant hearing loss is suspected in a child with OME. The results of the hearing test can help determine how to proceed, based on the hearing level noted for the better hearing ear.
You can manage children with hearing loss ≤20 dB and without speech, language, or developmental problems with watchful waiting. Children with hearing loss of 21 to 39 dB can be managed with watchful waiting or referred for surgery. If watchful waiting is pursued, there are interventions at home and at school that can help. These include speaking near the child, facing the child when speaking, and providing accommodations in school so the child sits closer to the teacher. Consider re-examination and repeat hearing tests every 3 to 6 months until the effusion has resolved or the child develops symptoms indicating surgical referral.
When hearing loss is ≥40 dB, the AAP/AAFP/AAOHNS guideline recommends that you make a referral for surgical evaluation (ALGORITHM).17