Applied Evidence
Richard E. Gray, DO
Heidi L. Gaddey, MD
Family Medicine Residency Program, University of Nebraska Medical Center and the 55th Medical Group, Offutt Air Force Base, Neb
heidi.gaddey@us.af.mil
The authors reported no potential conflict of interest relevant to this article. The views expressed here are those of the authors and do not reflect the official policy of the Department of the Air Force, the Department of Defense, or the US government.
Click here to view RADIOLOGY REPORT: Two radiologists offer 6 tips of the trade
Click here to view RADIOLOGY REPORT: 2 cases to test your skills

When patients present with acute nontraumatic abdominal pain, knowing what disorders and which imaging modalities to consider is essential. Let this article and handy table be your guide.
› Choose ultrasonography as the initial imaging test for patients with pain in the right upper quadrant. C
› Order computed tomography with contrast of the abdomen and/or pelvis for adults with acute pain of new onset in the right or left lower quadrant, or both. C
› Recommend ultrasound with graded compression as the initial imaging modality for children younger than 14 years who have acute right lower quadrant pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Harry L, age 54, presents with acute onset abdominal pain that began 2 days ago. He reports mild nausea but no vomiting, non-bloody diarrhea, and feeling feverish. The patient denies increased pain with movement.
If Mr. L were your patient, how would you proceed?
Although acute nontraumatic abdominal pain accounts for only about 1.5% of physician office visits, it is the cause of approximately 8% of visits—more than 11 million, a year—to US emergency departments.1,2 In most cases, the location of the pain, coupled with the patient history, physical exam, and clinical judgment, lead to the differential diagnosis and determines what type of imaging, if any, is needed.
Benign self-limiting causes of abdominal pain, such as constipation or gastroenteritis, may not require any imaging. However, if the patient has abdominal pain and fever, is older than age 65, or presents with peritoneal signs and symptoms, imaging will be a crucial diagnostic aid.3,4
With that in mind, the American College of Radiology (ACR) has developed a 9-point scoring criteria based on both the site and common causes of abdominal pain to determine the best imaging modality to use to rule in—or out—serious disease and conditions for which surgery is required. A rating of 1, 2, or 3 indicates that imaging is usually not appropriate; a rating of 4, 5, or 6 means the imaging test may be appropriate, and a rating of 7, 8, or 9 indicates that the recommended test is usually appropriate. The panel of experts who developed the scores considered the relative radiation level of each imaging modality, as well.5
In the text and TABLE3,6-12 that follow, you’ll find the most likely clinical diagnoses and the optimal tests for abdominal pain, based largely on where it hurts.
CASE 1 › Appendicitis: An 8-year-old girl presented with acute right lower quadrant pain and underwent an ultrasound (left), which showed a dilated ~2 cm (normal <6 mm) non-compressible appendix consistent with acute appendicitis. There was no significant free fluid within the right lower quadrant. Follow-up computed tomography (CT) scan (middle) with IV and oral contrast confirmed the dilated appendix with no evidence of perforation or abscess formation.
CASE 2 › Small bowel obstruction: A 54-year-old man sought care for abdominal pain and distention. A CT with IV and oral contrast (right) revealed multiple, fluid-filled dilated loops of small bowel (arrows) with bowel wall thickening, edema, and inflammatory stranding. The short segment of decreased enhancement (arrowhead) was consistent with bowel ischemia.
Right upper quadrant pain: Beware of acute biliary disease
Abdominal pain of the right upper quadrant (RUQ) is typically related to biliary, colonic, hepatic, or renal causes.12 Because of infection and the potential need for surgical intervention, untreated acute biliary disease can become life-threatening, particularly in the elderly.4
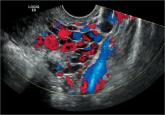
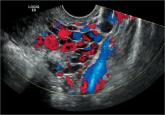
The ACR recommends ultrasound (US) as the initial imaging study for RUQ pain, regardless of whether the patient is febrile or has an elevated white blood cell count or a positive Murphy’s sign (demonstrated at youtube.com/watch?v=9L7N89sOSuc) (score=9). A 2012 meta-analysis found that US has a sensitivity of 81% and specificity of 83% for diagnosing acute cholecystitis.6
Although cholescintigraphy has a higher sensitivity and specificity (96% and 90%, respectively), US remains the initial study of choice because of its availability, study time, and the lack of ionizing radiation. For equivocal findings, computed tomography (CT), magnetic resonance imaging (MRI), and cholescintigraphy have similar levels of evidence.6
Epigastric/left upper quadrant pain: Consider pancreatits
Epigastric and left upper quadrant (LUQ) pain may have a gastric, biliary, pancreatic, vascular, renal, or cardiac etiology.12 The ACR criteria for testing depends on the type of pain suspected.
Pancreatitis. The Revised Atlanta Classification of Acute Pancreatitis requires 2 of the 3 classic criteria for a pancreatitis diagnosis: 1) abdominal pain suggestive of pancreatitis, 2) serum amylase and lipase levels ≥3 times the normal level, and 3) characteristic findings on imaging.13 The ACR recommends US as the initial imaging modality for suspected acute pancreatitis when it is the initial presentation, the patient has typical abdominal pain and increased serum amylase and lipase, and symptom onset was <48 to 72 hours before the patient sought care (score=9).7