Applied Evidence
Richard E. Gray, DO
Heidi L. Gaddey, MD
Family Medicine Residency Program, University of Nebraska Medical Center and the 55th Medical Group, Offutt Air Force Base, Neb
heidi.gaddey@us.af.mil
The authors reported no potential conflict of interest relevant to this article. The views expressed here are those of the authors and do not reflect the official policy of the Department of the Air Force, the Department of Defense, or the US government.
Click here to view RADIOLOGY REPORT: Two radiologists offer 6 tips of the trade
Click here to view RADIOLOGY REPORT: 2 cases to test your skills

Small bowel obstruction. When small bowel obstruction is suspected, CT of the abdomen and pelvis with contrast (score=9) is recommended. Oral contrast is not indicated if you suspect a high-grade obstruction, but may add functional information when only a partial or low-grade obstruction is suspected. The relative radiation level remains the same for both.11 For patients with pain and fever, postoperative or not, CT of the abdomen and pelvis with contrast is recommended (score=8).3
Mesenteric ischemia is associated with high morbidity and mortality rates (30%-90%).18,19 Acute mesenteric ischemia is most commonly secondary to embolism, followed by arterial thrombosis, non-occlusive ischemia, and less commonly, venous thrombosis.18 The typical presentation is pain out of proportion to the physical exam.19
In children with right lower quadrant pain suggestive of acute appendicitis, ultrasound is the first line imaging method due to its relatively high sensitivity and specificity and lack of ionizing radiation.
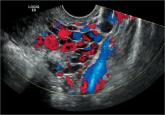
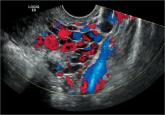
Differentiating mesenteric ischemia from other causes of acute abdominal pain can be difficult. Patients with chronic mesenteric ischemia present with postprandial abdominal pain, weight loss, and food avoidance. Although radiography is often the initial test ordered, a negative test does not rule out mesenteric ischemia. Therefore, the ACR recommends CT angiography (CTA) of the abdomen with contrast for the evaluation of both acute and chronic mesenteric ischemia (score=9). US can be useful for excluding other causes of abdominal pain, as well as ischemia related to venous occlusion, but it has a low sensitivity (70%-89%)18 overall and therefore is not recommended as the initial test for acute or chronic mesenteric ischemia.
Magnetic resonance angiography (MRA) has a high sensitivity and specificity for severe stenosis or origin occlusions of the superior mesenteric artery and celiac axis; however, its ability to determine distal embolism and non-occlusive ischemia, and the length and availability of this test limit its usefulness.18
When the patient is a child
Imaging for bilious vomiting in infants up to 3 months varies based on age. In the first week of life, radiography of the abdomen is the ACR’s recommended first-line test (score=9).20 An upper GI series or contrast enema are also options, but less preferred due to their increased radiation exposure.20
For infants between one week and 3 months of age, an upper GI series is the study of choice (score=9) and radiography of the abdomen is second line (score=5). An upper GI series is recommended to evaluate non-bilious, intermittent non-projectile vomiting in those from birth to 3 months.20 Projectile non-bilious vomiting should be evaluated with US of the abdomen.20
In children with RLQ pain suggestive of acute appendicitis, US is the first line imaging method due to its relatively high sensitivity and specificity and lack of ionizing radiation (score=9).10 If US is inconclusive, then CT of the abdomen and pelvis with IV contrast, but not oral or rectal contrast, is recommended (score=7). Although MRI is a non-radiating modality, it should be reserved for use only in specialized pediatric facilities due to lack of experience, increased cost, and the usual need for sedation.10
CASE › Mr. L’s vital signs demonstrated mild tachycardia and his body temperature was 100.5° F. His physical exam revealed significant tenderness to palpation in the LL Q, but no rebound or guarding. A CT scan with contrast of the abdomen revealed diverticulitis without abscess or perforation. The patient was managed with a clear liquid diet and told to return to the clinic 2 days later.
CORRESPONDENCE
Heidi L. Gaddey, MD, Family Medicine Residency Program, University of Nebraska Medical Center and the 55th Medical Group, 2501 Capehart Road, Offutt Air Force Base, NE 68113; heidi.gaddey@us.af.mil