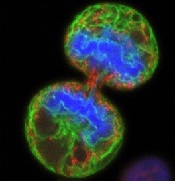
(endoplasmic reticulum in
green, mitochondria in red,
and chromosomes in blue)
Wellcome Images
The dynein-binding protein Lis1 is critical for hematopoietic stem cell (HSC) function and blood formation, according to a paper published in Nature Genetics.
Investigators found that Lis1 regulates asymmetric division of HSCs, ensuring the cells correctly differentiate to provide an adequate supply of new blood cells.
The research also indicated that Lis1 plays a key role in leukemias, as leukemic stem cells rely on the protein to regulate and sustain their growth.
“[Asymmetric division] is very important for the proper generation of all the cells needed for the development and function of many normal tissues,” said study author Tannishtha Reya, PhD, of the University of California, San Diego School of Medicine.
When cells divide, Lis1 controls orientation of the mitotic spindle, an apparatus of subcellular fibers that segregates chromosomes during cell division.
“During division, the spindle is attached to a particular point on the cell membrane, which also determines the axis along which the cell will divide,” Dr Reya said. “Because proteins are not evenly distributed throughout the cell, the axis of division, in turn, determines the types and amounts of proteins that get distributed to each daughter cell.”
When the investigators deleted Lis1 from mouse HSCs, differentiation was radically altered. Asymmetric division increased and accelerated differentiation.
This led to an oversupply of specialized cells and an ever-diminishing reserve of undifferentiated stem cells, which eventually resulted in a bloodless mouse.
“What we found was that a large part of the defect in blood formation was due to a failure of stem cells to expand,” Dr Reya said.
“Instead of undergoing symmetric divisions to generate 2 stem cell daughters, they predominantly underwent asymmetric division to generate more specialized cells. As a result, the mice were unable to generate enough stem cells to sustain blood cell production.”
The investigators next looked at how leukemic stem cells in mice behaved when the Lis1 signaling pathway was blocked. And the team discovered that these cells also lost the ability to renew and propagate.
“In this sense, the effect Lis1 has on leukemic self-renewal parallels its role in normal stem cell self-renewal,” Dr Reya said.
She added that these findings shed new light on the fundamental regulators of cell growth, both in normal development and in cancer.
“Our work shows that elimination of Lis1 potently inhibits cancer growth and identifies Lis1 and other regulators of protein inheritance as a new class of molecules that could be targeted in cancer therapy,” she said.
However, it remains to be seen whether inhibiting Lis1 in cancer cells would produce unacceptable consequences in normal cells as well.
“Agents that target Lis1 might be more specific and less toxic [than chemotherapy],” Dr Reya said, “which would give them significant clinical value.”

