THE CASE
A 14-year-old Caucasian boy presented to our clinic with a complaint of left anterior hip pain. The patient had been running during a flag football match when he suddenly developed a sharp, stabbing pain in his left hip. He said he felt a “pop” in his left groin while his left foot was planted and he was cutting to the right. The patient said this was followed by worsening pain with ambulation and hip flexion.
The patient had considerable difficulty walking into the exam room. On physical examination, he had significant tenderness to palpation along the anteromedial thigh and groin. The patient’s strength was 1/5 with left hip flexion. There was apparent muscle firing, but no significant leg movement. He had full passive range of motion and there was no soft-tissue swelling, erythema, or other integumentary changes.
THE DIAGNOSIS
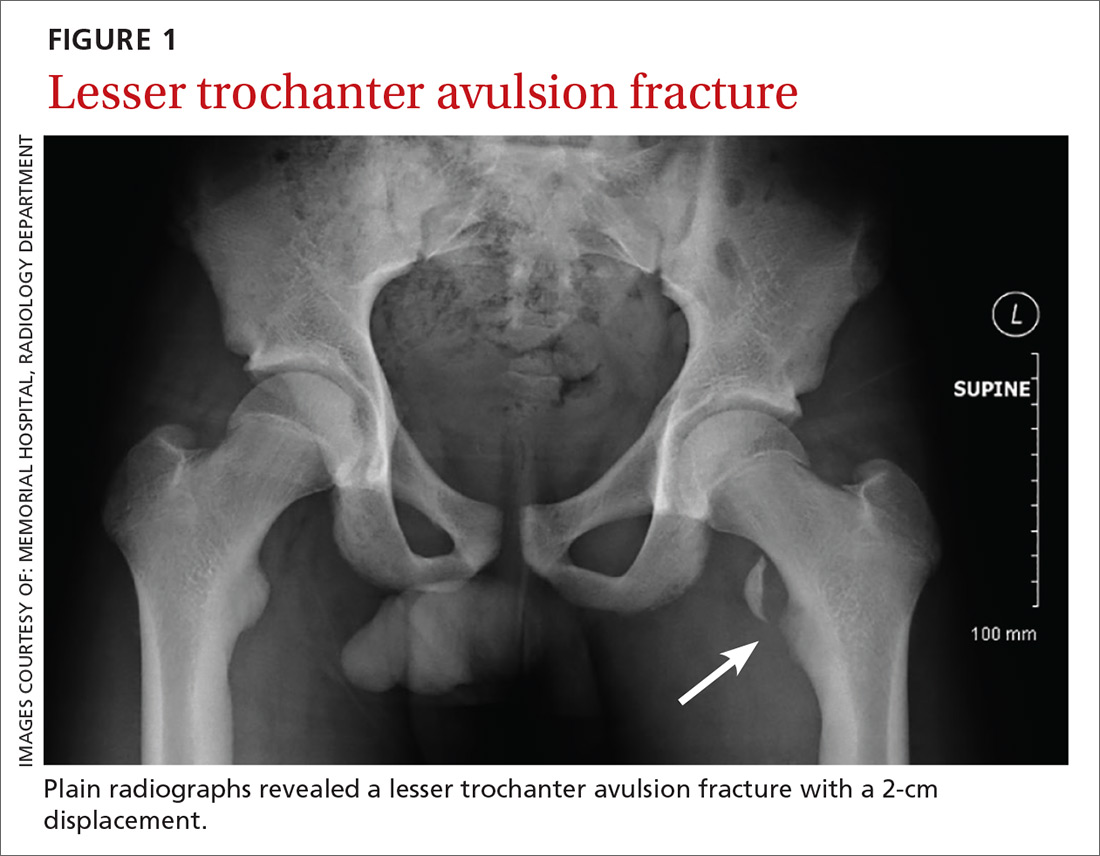
Plain radiographs revealed a lesser trochanter avulsion fracture with a 2-cm displacement (FIGURE 1).
DISCUSSION
Pelvic and proximal femur avulsion fractures tend to occur during the second decade of life.1,2 They’re more frequently seen in boys and adolescent athletes, especially those involved in soccer and gymnastics.3,4
Anterior superior iliac spine (ASIS), ischial tuberosity (IT), and anterior inferior iliac spine (AIIS) avulsion fractures are more prevalent,4 while lesser trochanter avulsion fractures are more rare. In one review of 1126 children with femoral neck and proximal 1/3 femoral shaft fractures, only 3 of them had lesser trochanter avulsion fractures.5
Clinical presentation. Presenting symptoms of lesser trochanter avulsion fractures can be vague, but are usually localized to the groin and medial hip region. Patients will demonstrate pain and weakness with hip flexion.3,6 There may be signs of inflammation, tenderness, and ecchymosis near the site of injury.
On physical exam, a positive Ludloff sign helps localize the injury to the iliopsoas muscle, which inserts at the lesser trochanter and is involved in hip flexion.3,6,7 The Ludloff test is performed by flexing the patient’s hip while he/she is in a seated position.
BIOMECHANICS OF AVULSION FRACTURES
Perhaps surprisingly, the majority of avulsion injuries in children and adolescents are the result of non-contact athletic movement and indirect trauma.4 In children, muscles and tendons are often stronger than their bones,7 and physes—structurally weak regions—are particularly predisposed to fractures.2,4,6
The mechanism of injury in children and adolescents is commonly a sudden, forceful contraction of the iliopsoas muscle.6,7 While similar movement in adults will produce tendon sprains and muscle strains, children often experience a complete avulsion fracture.7 So uncommon are these fractures among adults that an adult patient presenting with one should receive further work-up for underlying pathology such as malignancy.8,9
While other hip and femur avulsion fractures in children and adolescents involve different muscle groups, the etiologic mechanism—forceful muscle contraction—is usually the same.2,4,7 IT injuries are often seen with sudden, aggressive lengthening of the hamstring muscles, whereas injuries to the ASIS and AIIS are the result of abrupt eccentric contraction of hip extensor muscles while the knee is flexed.4
DIFFERENTIAL DIAGNOSIS
There are several entities that can mimic a lesser trochanter avulsion fracture including Legg-Calve-Perthes disease (LCPD), slipped capital femoral epiphysis (SCFE), snapping hip with the iliofemoral ligament, iliopsoas tendonitis, referred pain from the gastrointestinal region, and a genito-urologic etiology.1,7,10 The work-up and treatment for these alternative diagnoses are quite different and can lead to unnecessary testing.
Diagnostic studies. Physical exam findings of severe pain and reduced strength are clear indications for obtaining baseline imaging. Baseline radiographs are key to the diagnosis of avulsion fractures. They help differentiate between more benign fractures, such as a nondisplaced avulsion fracture, and more substantial conditions, such as LCPD and SCFE, which require significantly different approaches to treatment and follow-up.1,7
Anteroposterior, oblique, and axial views of the pelvis all assist in assessing avulsion fractures radiographically.3,4,7 In the event that an avulsion fracture is not radiographically visible, but is still suspected, additional imaging should be obtained.10 A computerized tomography (CT) scan is an appropriate follow-up, given its meticulous detail of bony anatomy.3,10 Alternatively, if physes have yet to ossify or there are concerns about soft tissue injury, magnetic resonance imaging can be useful.3,7,10