Additional insights from the UKPDS
Hypoglycemia in type 2 diabetes has not received rigorous attention in clinical trials. However, the United Kingdom Prospective Diabetes Study (UKPDS) was a large longitudinal trial in type 2 diabetes that included hypoglycemia as an outcome measure and thus provides some helpful information.
Events with insulin>sulfonylureas>diet. The 6-year follow-up revealed that the cumulative proportion of patients reporting 1 or more hypoglycemic events (of any type) was 76% for those using insulin, 45% among those taking sulfonylureas, and 3% for those on diet alone. Expressed as events per patient year, this was 37%, 17%, and 0.9%, respectively. When only “major” events (those requiring third-party assistance or hospital admission) were considered, the proportion of patients per year reporting 1 or more such events, was 2.3% for insulin, 0.7% for sulfonylureas, and 0.03% for diet alone. The cumulative proportion over 6 years was 3.3% of participants using sulfonylureas, 11.2% of those using insulin, and 0.15% of those on diet therapy.8
Metformin increases risk. The cumulative proportion of obese patients reporting any hypoglycemic event was 17.6% for those taking metformin vs 2.8% for those on diet. Severe hypoglycemia (as defined earlier) occurred in 2.4% of participants using metformin compared with 0.4% of those on diet therapy.8
Findings from other studies
Interestingly, in a recent systematic review of randomized controlled trials comparing insulin monotherapy with insulin plus oral antidiabetic agents, 13 of 14 studies reporting hypoglycemia demonstrated no difference in events.14
The occurrence of hypoglycemia among patients on metformin monotherapy in the UKPDS study is notable since, theoretically, hypoglycemia should not occur with agents whose mechanisms of action do not increase insulin secretion (biguanides, thiazolidinediones [TZDs], or α-glucosidase inhibitors),1 Since newer classes such as TZDs, α-glucosidase inhibitors, and meglitinides were not available when UKPDS was initiated, the trial does not provide data on these classes.
In a small comparative study of insulin combined with either metformin or a TZD, it appeared that metformin combination was associated with fewer occurrences of hypoglycemia; however, the small patient sample limits generalizability of the finding.15
How hypoglycemia occurs
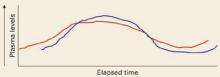
Normally, as blood glucose levels (red) rise, insulin secretion increases, circulating insulin levels (blue) rise, and hepatic glucose production is inhibited. As glucose is disposed and circulating levels decrease due to insulin action, insulin levels then drop and hepatic glucose production begins again.
Hypoglycemia in diabetes can result from an excess of endogenous or exogenous insulin (iatrogenic hypoglycemia). In healthy patients, high insulin and falling glucose levels suppress insulin production and stimulate a hormone-mediated burst of glucose production. In patients with diabetes, the loss of physiologic control of insulin secretion coupled with exogenous administration of insulin or insulin secretagogues can interfere with the normal physiologic response to low blood glucose levels, resulting in hypoglycemia.1
With intense insulin regimens, the incidence of hypoglycemia can be as high as 30%, in contrast to 12% for patients treated with diet alone and 16% for those taking oral agents.6
With secretagogues, it has been suggested that the incidence of hypoglycemia is higher with the older, longer acting sulfonylurea agents.1,6,16-19 Although populationbased data on hypoglycemic rates associated with combination therapy with oral antidiabetic agents are not available, numerous clinical studies have reported rates of 10% to 20% for any hypoglycemic event.20-23
Heightening patient awareness, and yours
Because the signs of hypoglycemia vary considerably among individuals, they can easily be missed.3 In addition, repeated episodes of hypoglycemia can alter the normal regulatory responses and diminish the most important signs of a drop in glucose levels.1,2,24,25 The loss of the physiologic warning signs is thought to stem from dampening and eventual loss of the neuroadrenal response to low glucose levels in the brain (FIGURE 1). A vicious cycle is set up, whereby reduction in the neurogenic response attenuates hypoglycemic symptoms, causing more episodes to occur and become more severe as they are repeated. This cycle can be broken, and the normal physiologic response restored, if hypoglycemic events can be avoided for just a few weeks.2,26
Key points for patients. The main strategy for managing hypoglycemia is educating patients about the early symptoms of hypoglycemia and how to self-treat when they occur. Reinforce the need to time meals consistently and to limit the amount of carbohydrate ingested.
Advise patients to monitor blood glucose levels frequently, and to learn to relate a drop in glucose levels to hypoglycemic symptoms.2
Counsel patients to eat a snack or, preferably, drink fruit juice to counteract hypoglycemia. Patients may also carry glucose tablets, which are convenient and less tempting than candy.27