Glucagon is indicated for severe cases.
Whenever possible, a patient’s family members (particularly in the case of children) should be educated too.
Ask regularly about episodes. Finally, act to identify problems by querying patients and family members at every visit about hypoglycemia episodes, probing for information about awareness, severity and timing of the episodes, and how these events relate to dosing, meals, and activities.27 If hypoglycemia recurs, analyze the dosing regimen and consider flexible insulin dosing.1
Anti-hypoglycemia strategies for each new phase of therapy
As the course of diabetes therapy moves, typically, from oral medications to insulin to combination regimens, drug selections can be made in part to reduce the risk of hypoglycemia.
Oral agents: Insulin sensitizers, newer agents generally better
As noted earlier, among oral agents, insulin sensitizers are generally thought to have lower rates of hypoglycemia.
Newer sulfonylureas such as glimepiride and the rapid-acting meglitinides may also cause fewer hypoglycemic events.
Given the progressive decline of endogenous insulin secretion, combination therapy with secretagogues or insulin is eventually required for most patients.
Insulin analogs
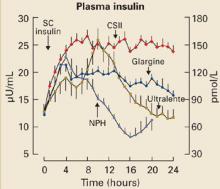
A number of rapid-, short-, intermediateand long-acting insulin analogs have been introduced, and many of them make it possible to mimic different phases of physiologic insulin secretion (FIGURE 2). One of the newer analogs less likely to cause hypoglycemia is glargine, a long-acting insulin with a steady, relatively consistent action profile over a 24-hour period, closely mimicking normal basal pancreatic insulin secretion.28
FIGURE 2
Plasma insulin levels with newer analogs
N=20 type 1 diabetic patients; mean±SE
CSII, continuous subcutaneous insulin infusion; NPH, neutral protamine Hagedorn.
Copyright © 2000 American Diabetes Association. From Diabetes 2000; 49:2142–2148.28 Reprinted with permission from American Diabetes Association.
TABLE 2
Strategies for avoiding and addressing hypoglycemia
|
Insulin mixtures helpful when meal times guaranteed
Other insulins include mixtures of regular insulin and long-acting insulin available in split mixed or premixed formulations. These mixtures are intended to cover insulin peaks at mealtimes with twice-daily administration.
Mixed insulin formulations are often perceived as relatively convenient and simple to use, but they require meals to be taken within set time frames, without a great deal of flexibility. Since the ratios of the insulin components are fixed, and designed to work with meals consumed on a fixed schedule, hypoglycemia can occur if patients miss a meal. In addition, the time-activity profile of the insulin may not match the postprandial glucose peak even if the meal is consumed, and will increase the chance of postprandial hypoglycemia.
Basal insulin plus oral regimens
For patients with type 2 diabetes, adding basal insulin to oral regimens can significantly improve glycemic control. Ideally, basal insulin therapy provides a sustained and relatively constant concentration of insulin throughout the day. In the past, neutral protamine Hagedorn (NPH) insulin, a longer-acting insulin, was used for basal insulin therapy, and regular insulin was used to cover prandial insulin needs. Ultralente, also used as a basal insulin, has a relatively unpredictable timeactivity profile.28
Insulin glargine superior to NPH. In a recent clinical trial, patients with type 2 diabetes whose glucose levels were inadequately controlled on oral antidiabetic medications were given bedtime insulin glargine or NPH insulin.29 The insulin doses were titrated using a simple algorithm targeting a fasting plasma glucose (FPG) of ≤100 mg/dL to reach recommended glycosylated hemoglobin (Hb A1c) levels. Though no significant difference in glycemic control was found between insulin glargine and NPH insulin, significantly fewer hypoglycemic episodes occurred with insulin glargine therapy. The 24-hour distribution per patient-year of hypoglycemia for glargine vs NPH is shown in FIGURE 3.
Specifically, nearly 25% more patients treated with insulin glargine than with NPH insulin reached target Hb A1c levels of ≤7.0% without nocturnal hypoglycemia. Moreover, the overall incidence of any hypoglycemic event (eg, plasma-referenced glucose ≤72 mg/dL) and severe hypoglycemia (eg, patient required assistance of another person, and had a glucose level <56 mg/dL or prompt recovery after glucose or glucagons) was lower with insulin glargine than with NPH insulin. Results from other studies and a recent metaanalysis have been similar.30-32